When you hear serotonin norepinephrine reuptake inhibitors, a class of antidepressants that increase levels of both serotonin and norepinephrine in the brain. Also known as SNRIs, they’re often prescribed when SSRIs don’t work well enough—or when someone needs help with both mood and physical pain. Unlike older antidepressants, SNRIs don’t just lift your mood; they can ease nerve pain, fatigue, and even some types of headaches. That’s why doctors reach for them for depression, anxiety, fibromyalgia, and chronic back pain—not just sadness.
But SNRIs aren’t magic. They work by blocking the brain from reabsorbing serotonin and norepinephrine, letting more of these chemicals hang around where they’re needed. That sounds simple, but your body doesn’t always respond the same way. Some people feel better in weeks; others get headaches, nausea, or trouble sleeping before they improve. And if you’re already on other meds—like painkillers, blood pressure drugs, or even kombucha (yes, really)—you could be at risk for dangerous interactions. That’s why knowing what else is in your medicine cabinet matters just as much as the SNRI itself.
Not everyone needs an SNRI. For some, switching to a different antidepressant, a medication used to treat depression and sometimes anxiety or chronic pain. Also known as SSRIs or tricyclics, it can be a safer or more effective choice makes more sense. Others find relief with therapy, exercise, or non-drug approaches. Even when SNRIs are the right call, the brand name isn’t what matters—it’s the active ingredient. You might pay $200 for a brand, or $15 for a generic version that does the same job. And if you’ve ever had a weird reaction to a generic pill, you’re not alone. Small differences in fillers or coatings can trigger side effects in sensitive people, especially with drugs that have a narrow therapeutic window.
What you won’t find in most doctor’s offices is the full picture. Why does one person get dizzy on venlafaxine but feel fine on duloxetine? Why do some people report weight gain while others lose weight? The answers aren’t always in the pamphlet. That’s why real-world experiences—from people managing chronic pain, dealing with anxiety after childbirth, or trying to quit cold turkey—matter more than clinical trials. Below, you’ll find honest takes on SNRIs, what they actually do to your body, how they mix with other meds, and what to do when they don’t work—or make things worse.
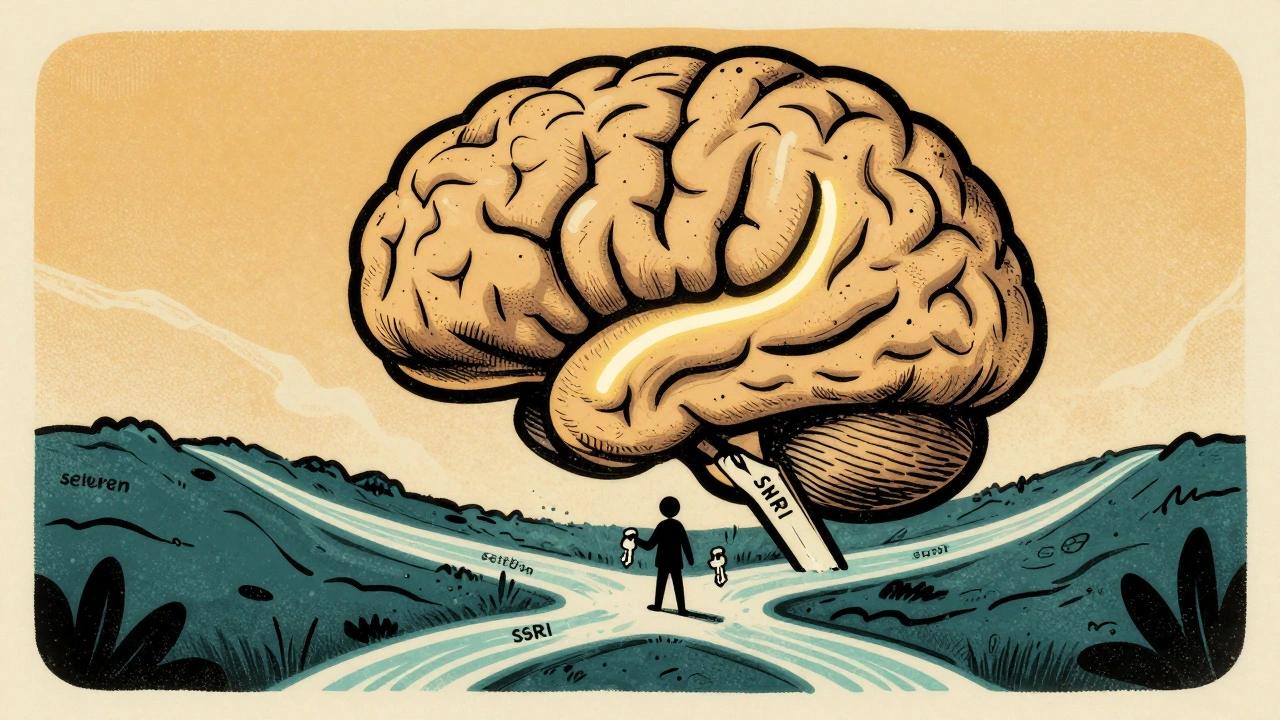
SNRI medications offer a dual-action approach to treating depression and chronic pain by boosting serotonin and norepinephrine. Learn how they compare to SSRIs, their real-world effectiveness, side effects, and why they're a key option for treatment-resistant cases.

The best time to take statins isn't about night or morning-it's about consistency. Learn how statin timing affects side effects and cholesterol lowering, and why adherence beats clock time.

Sedating antihistamines like diphenhydramine significantly increase fall risk in older adults. Learn why first-generation options are dangerous, which safer alternatives exist, and practical steps to prevent falls through medication changes and home safety.

Learn practical ways to boost iron, B12, calcium, vitamin D and zinc absorption on vegetarian and vegan diets with food combos, cooking hacks, and gut‑health tips.

Compare Waklert (armodafinil) with modafinil, Adrafinil, Adderall, and natural alternatives to find the safest, most effective option for focus and alertness. Learn what works, what doesn’t, and why.
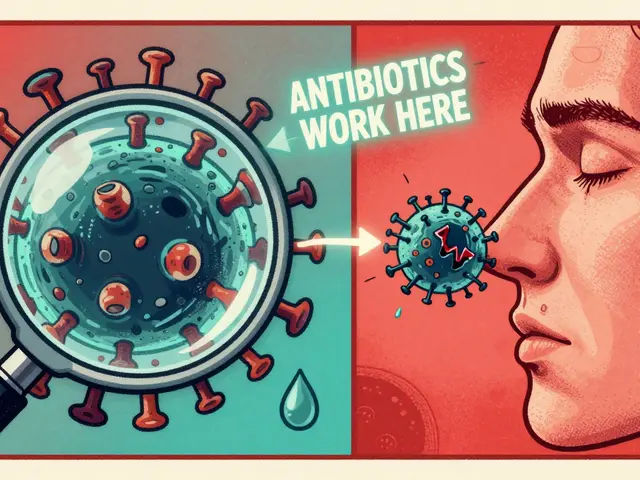
Learn how to tell bacterial and viral infections apart, why antibiotics don't work on viruses, and what treatments actually help. Stop unnecessary antibiotic use and protect yourself from superbugs.