When you take certain medications, your body’s ability to handle heat changes—sometimes dangerously. These are called heat exposure drugs, medications that impair your body’s cooling mechanisms or increase sensitivity to high temperatures. Also known as thermoregulatory-interfering drugs, they don’t just cause discomfort—they can lead to heat exhaustion, heat stroke, or even death if ignored. It’s not just about sweating more. These drugs interfere with how your body regulates temperature, slows down fluid loss, or blocks the signals that tell you you’re overheating.
Many of these drugs fall into common categories. anticholinergics, medications that block acetylcholine, a key neurotransmitter for sweat production, are a big one. Think diphenhydramine in allergy pills or amitriptyline for pain and sleep. They stop your sweat glands from working, so your body can’t cool down. Then there are diuretics, drugs like hydrochlorothiazide that make you pee more to lower blood pressure. They drain your fluids, and when it’s hot, that dehydration hits faster. Even some antidepressants, blood pressure meds like ramipril, and stimulants used for focus can mess with your body’s heat response. You might not realize it until you’re dizzy, nauseous, or confused.
Heat exposure drugs don’t act alone. They often team up with other risks—like being over 65, having heart disease, or spending time outside without water. A 70-year-old on a diuretic for high blood pressure who takes an antihistamine for allergies? That’s a recipe for trouble on a 90-degree day. The problem isn’t the drug itself—it’s the combination of the drug, the weather, and your body’s reduced ability to adapt. Many people think, "I’ve taken this pill for years," but heat changes everything. Your body’s limits shrink when the temperature rises.
What can you do? First, know your meds. Check your pill bottles. If you’re on anything for blood pressure, depression, allergies, or bladder control, ask your doctor if it affects heat tolerance. Second, stay hydrated—not just with water, but with electrolytes if you’re sweating a lot. Third, avoid the sun during peak hours. Wear light clothes. Use fans or AC. If you feel lightheaded, nauseous, or unusually tired in the heat, get indoors immediately. Don’t wait for a heat stroke to happen.
Below, you’ll find real-world guides on how specific medications interact with heat, what alternatives exist, and how to manage your health safely when temperatures climb. Whether you’re on a diuretic, an anticholinergic, or just worried about your meds in summer, these posts give you the facts—not guesses. No fluff. Just what you need to protect yourself.
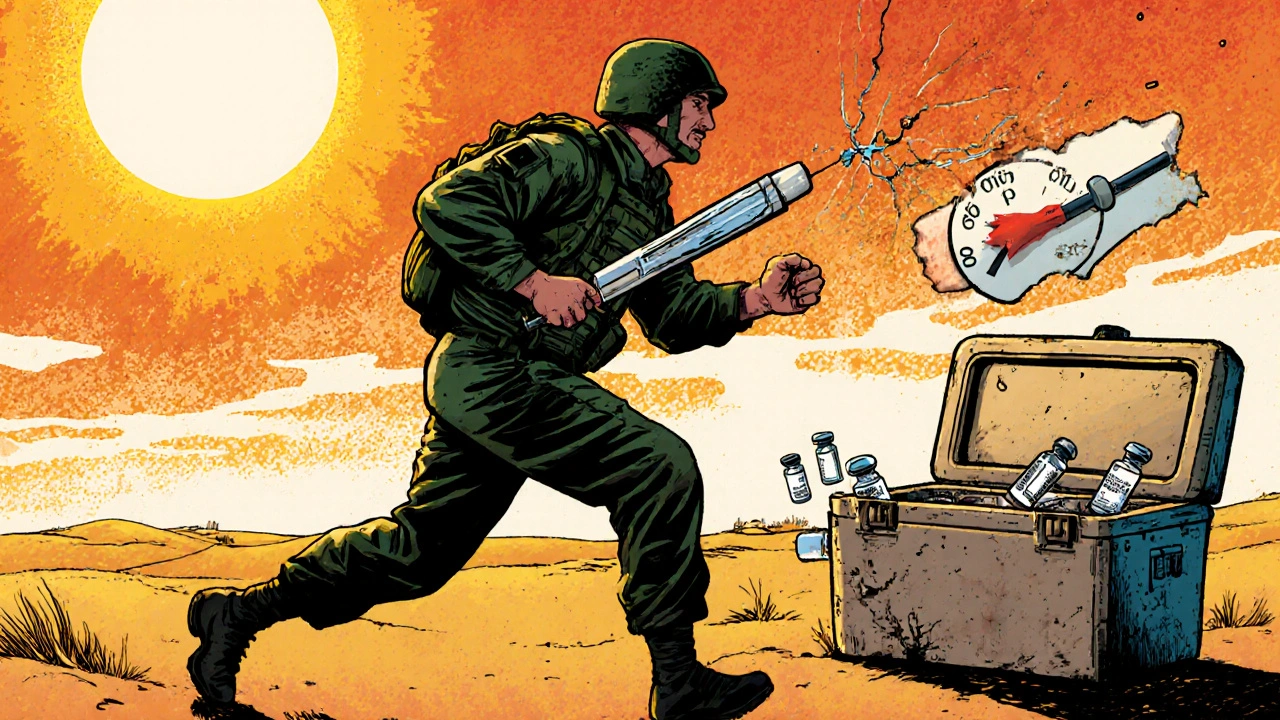
Military deployment exposes medications to extreme heat, storage failures, and access delays that can render life-saving drugs ineffective. From vaccines to insulin, improper storage threatens soldier readiness-and the military is racing to fix it.

Natrise (tolvaptan) raises sodium levels fast but carries liver risks and high costs. Learn how fluid restriction, urea, demeclocycline, and salt tablets compare as safer, cheaper alternatives for hyponatremia.
Warfarin and DOACs are both blood thinners used to prevent clots, but DOACs are now preferred for most patients due to better safety, fewer interactions, and no need for regular blood tests. Learn the key differences and what to do in an emergency.
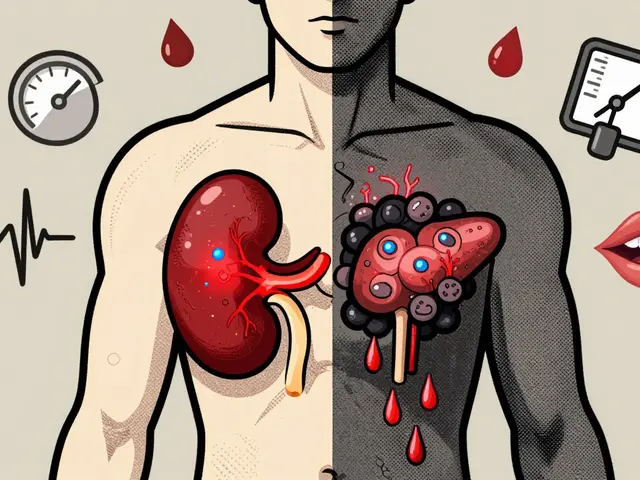
Cyclosporine and tacrolimus are essential for transplant patients but come with serious side effects like kidney damage, tremors, and diabetes. Learn how these drugs compare, what to watch for, and how doctors are now reducing their use to improve long-term health.

A clear comparison of Cleocin Gel (clindamycin) with other topical acne treatments, covering how they work, price, side effects, and tips for choosing the best option.
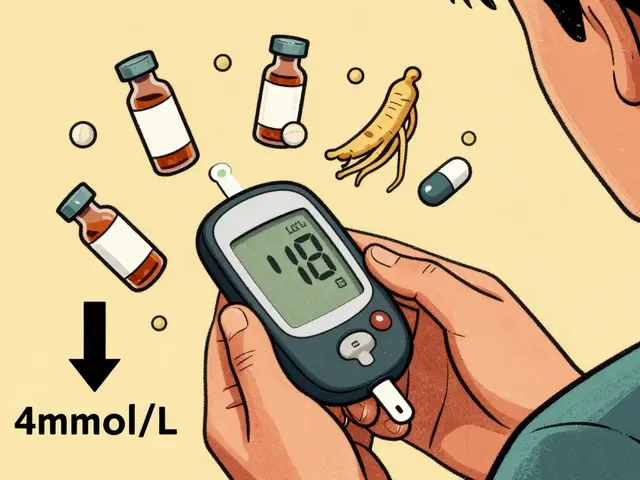
Ginseng may help lower blood sugar in type 2 diabetes, but it can dangerously interact with insulin and oral meds. Learn how to monitor your levels, avoid risks, and use it safely if approved by your doctor.