When your sodium levels drop too low, it’s not just a lab number-it’s fatigue, confusion, nausea, and sometimes seizures. Hyponatremia doesn’t always have a simple fix, and for many, Natrise (tolvaptan) becomes a go-to option. But it’s not the only one. If you’re weighing Natrise against other treatments, you’re asking the right question. Not all drugs work the same for everyone, and side effects, cost, and long-term safety matter just as much as how well it raises sodium.
What Natrise (Tolvaptan) Actually Does
Natrise is the brand name for tolvaptan, a vasopressin receptor antagonist. It works by blocking the hormone that tells your kidneys to hold onto water. When that signal is cut off, your body flushes out excess fluid without losing sodium. This makes it especially useful for hyponatremia caused by SIADH (syndrome of inappropriate antidiuretic hormone secretion), heart failure, or liver cirrhosis.
The FDA approved Natrise in 2009 specifically for low sodium due to SIADH. In clinical trials, patients saw sodium levels rise by an average of 4-6 mEq/L within 24-48 hours. That’s fast-and critical when symptoms are severe. But it’s not a cure. You need to keep taking it, and you need monitoring. Sodium can rebound if you stop too soon.
Why People Look for Alternatives to Natrise
Many patients start on Natrise and quickly realize it’s not ideal. The biggest complaints? Dry mouth, thirst, frequent urination, and liver enzyme spikes. About 1 in 10 people experience elevated liver enzymes, and in rare cases, that leads to serious liver damage. The FDA even issued a boxed warning for this.
Cost is another hurdle. A 30-day supply of Natrise can run over $1,500 without insurance. Even with coverage, copays often hit $200+. For someone managing a chronic condition, that adds up fast.
Then there’s the daily routine. You have to take it once a day, on an empty stomach, and avoid grapefruit juice. Missing a dose or eating the wrong thing can reduce effectiveness. For older adults or those on multiple meds, that’s a lot to manage.
Alternative #1: Fluid Restriction
Before drugs, doctors often started with one simple fix: drink less water. For mild hyponatremia, especially in SIADH, cutting fluid intake to 800-1,200 mL per day can slowly normalize sodium. It’s free, has no side effects, and doesn’t interact with other meds.
But it’s hard. Thirst doesn’t care about your doctor’s orders. People with SIADH often feel constantly thirsty, and restricting fluids feels like punishment. Studies show only about 40% of patients stick with it long-term. It works best for stable, mild cases-not emergencies.
Alternative #2: Demeclocycline
This antibiotic, originally used for acne and infections, has a side effect that turns out to be useful: it makes the kidneys less responsive to vasopressin. That means more water gets flushed out-similar to Natrise, but slower.
Demeclocycline is cheap. A month’s supply costs under $50. It’s been used for decades and is well-studied in SIADH. But it’s not fast. It can take 3-7 days to see sodium rise. It also causes sun sensitivity, nausea, and, rarely, kidney issues. You can’t use it if you’re pregnant or have liver disease. And because it’s an antibiotic, long-term use may disrupt gut bacteria.
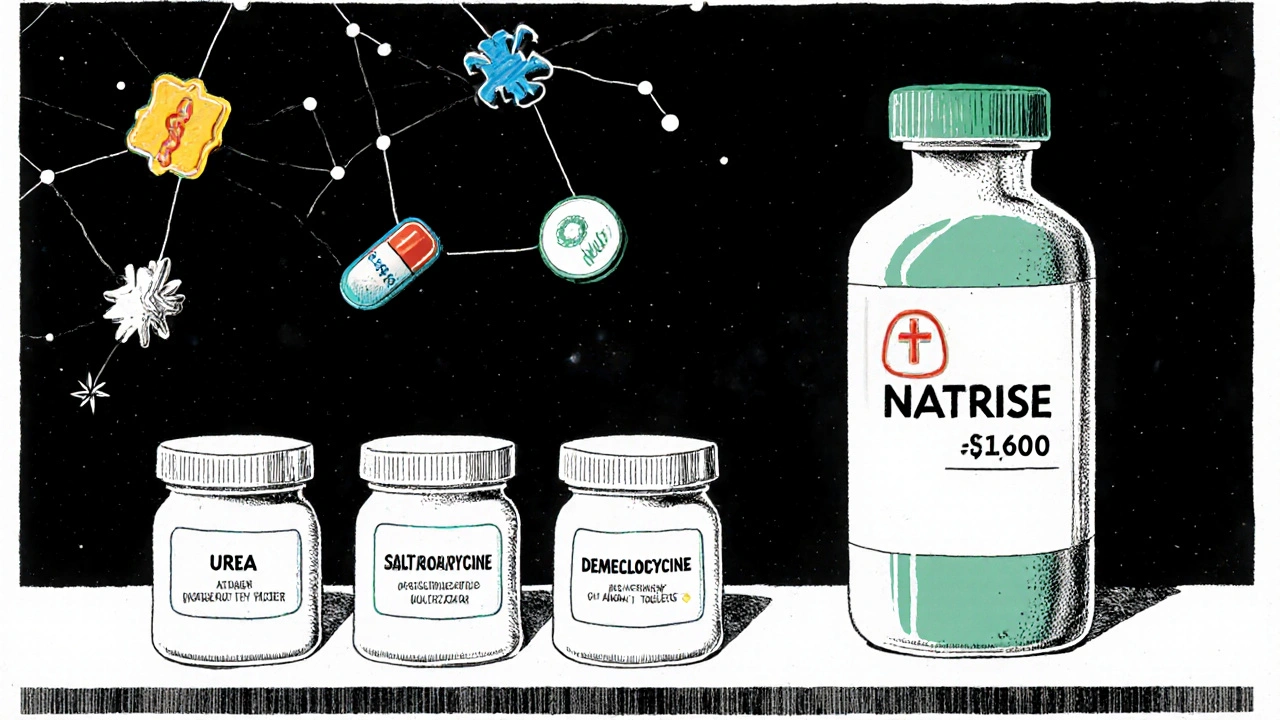
Alternative #3: Urea
Urea isn’t a drug you find at your local pharmacy-it’s a natural compound your body already makes. In medical form, it’s prescribed as a powder to mix with water. It works by increasing the osmotic pressure in your kidneys, pulling water out without affecting sodium.
It’s not FDA-approved for hyponatremia in the U.S., but it’s widely used in Europe and Canada. Studies show it raises sodium as effectively as tolvaptan, with fewer liver risks. Side effects? Bitter taste, bloating, and occasional stomach upset. Some patients mix it with juice to mask the flavor.
It’s affordable-around $100 a month-and doesn’t interact with most medications. It’s also safe for people with liver problems, making it a top choice for cirrhosis-related hyponatremia.
Alternative #4: Vaptans (Conivaptan)
Conivaptan is another vasopressin blocker, but it’s given intravenously. It’s only approved for hospital use in patients with severe hyponatremia who need rapid correction. You won’t take this at home.
It works faster than Natrise-sometimes within hours. But it’s not practical for long-term use. You need IV access, constant monitoring, and a hospital bed. It’s also expensive and carries the same liver risk as tolvaptan. For most people, it’s a bridge-not a solution.
Alternative #5: Salt Tablets and Hypertonic Saline
For acute, symptomatic hyponatremia, doctors sometimes use hypertonic saline (3% NaCl) through an IV. This is emergency care. It’s not for daily use.
Oral salt tablets (like NaCl 1 g tablets) are sometimes used for chronic cases, especially if fluid restriction isn’t enough. They’re cheap and easy. But they can cause high blood pressure, fluid retention, and heart strain if overused. They’re not a standalone fix-they’re usually paired with other treatments.
Comparison Table: Natrise vs Alternatives
| Treatment | Speed of Action | Cost (Monthly) | Common Side Effects | Best For | Liver Risk |
|---|---|---|---|---|---|
| Natrise (Tolvaptan) | 1-2 days | $1,200-$1,800 | Thirst, dry mouth, frequent urination | SIADH, stable chronic cases | High (boxed warning) |
| Fluid Restriction | Days to weeks | $0 | Dehydration, fatigue | Mild SIADH, elderly | None |
| Demeclocycline | 3-7 days | $30-$60 | Sun sensitivity, nausea | Chronic SIADH, low budget | Low |
| Urea | 2-5 days | $80-$120 | Bitter taste, bloating | Cirrhosis, liver patients | None |
| Conivaptan (IV) | Hours | $1,000-$2,000 (per admission) | Infusion reactions, low blood pressure | Emergency hospital use | High |
| Salt Tablets | 1-3 days | $10-$20 | High BP, fluid overload | Mild cases, adjunct therapy | None |
Who Should Avoid Natrise
Natrise isn’t right for everyone. Avoid it if you:
- Have severe liver disease (Child-Pugh Class C)
- Are allergic to tolvaptan or any of its ingredients
- Can’t drink enough fluids to replace what you’re losing
- Are taking strong CYP3A4 inhibitors like ketoconazole or clarithromycin (they spike tolvaptan levels)
- Have an inability to sense thirst or communicate symptoms (like advanced dementia)
These aren’t just warnings-they’re red flags. One study in the Journal of the American Society of Nephrology found that 18% of patients on Natrise had liver enzyme spikes within the first month. Half of those cases reversed after stopping the drug, but the risk isn’t worth it if you have other options.
What to Ask Your Doctor
If you’re on Natrise-or thinking about it-here’s what to bring up:
- "Is my hyponatremia caused by SIADH, heart failure, or something else?" (The cause changes the best treatment.)
- "Can we try fluid restriction or urea first?"
- "What’s my liver function history? Should we check enzymes monthly?"
- "Is there a generic version of tolvaptan available?" (There isn’t-yet.)
- "If I can’t afford this, what’s the next safest option?"
Don’t assume Natrise is the only answer. Many doctors prescribe it because it’s fast and FDA-approved. But if you’re stable, older, or on a budget, alternatives might be safer and just as effective.
Real-World Experience
One 72-year-old woman with SIADH from lung cancer tried Natrise for six weeks. Her sodium went from 128 to 136-but she couldn’t sleep because she was constantly thirsty. Her liver enzymes jumped 3x. She switched to urea powder. Within two weeks, her sodium stayed steady at 134. No thirst, no liver issues, and her monthly cost dropped from $1,600 to $95.
Another patient, a 58-year-old with heart failure, used salt tablets along with mild fluid restriction. His sodium stayed above 130 for over a year. He didn’t need any prescription drugs.
There’s no one-size-fits-all. Your body, your condition, your budget, and your tolerance for side effects all matter.
Bottom Line
Natrise works-but it’s not the only option, and it’s not always the best. For many, fluid restriction, urea, or even salt tablets offer similar results with fewer risks and lower cost. If you’re on Natrise and feeling side effects, don’t just tough it out. Talk to your doctor about alternatives. Your liver, your wallet, and your quality of life will thank you.
Can I take Natrise with other medications?
You should avoid Natrise with strong CYP3A4 inhibitors like ketoconazole, itraconazole, clarithromycin, or ritonavir. These drugs can cause tolvaptan levels to build up dangerously in your blood. Always tell your doctor about every medication, supplement, or herb you take. Even over-the-counter painkillers like ibuprofen can affect sodium levels and interact indirectly.
How long do I need to take Natrise?
There’s no set time. Some people take it for months, others for years. It depends on the cause of your hyponatremia. If your condition improves-like if a tumor causing SIADH is removed-you may be able to stop. But stopping too soon can cause sodium to drop again. Never stop without your doctor’s guidance.
Is there a generic version of Natrise?
No, there is no generic tolvaptan available in the U.S. as of 2025. The patent expired in 2023, but no manufacturer has launched a generic version yet. This is why the cost remains high. Some patients get it from Canadian pharmacies, but that’s not legal or safe without medical oversight.
Can I drink alcohol while taking Natrise?
It’s not recommended. Alcohol can lower sodium levels and worsen hyponatremia. It also increases dehydration risk, which can make side effects like dizziness or confusion worse. Even small amounts can interfere with how well Natrise works. If you drink, talk to your doctor about safe limits-or avoid it entirely.
What happens if I miss a dose of Natrise?
If you miss a dose, take it as soon as you remember-but only if it’s within 12 hours of your usual time. If it’s been longer, skip the missed dose and take your next one at the regular time. Don’t double up. Missing doses can cause sodium levels to drop again, especially if your condition is unstable. Keep a daily log to track your doses.
Are there natural ways to raise sodium levels?
Yes, but only in mild cases. Eating more salt (like adding salt to meals or using salted snacks) can help, but it’s not enough on its own. The real key is reducing water intake and avoiding sports drinks, beer, or excessive fluids. For severe hyponatremia, natural methods won’t work. Always pair dietary changes with medical supervision.
Does Natrise cause weight loss?
Yes, many people lose weight on Natrise-not from fat loss, but from water loss. It’s common to drop 2-5 pounds in the first week as your body flushes excess fluid. This is normal and expected. But if you lose more than 2 pounds per day or feel dizzy, weak, or lightheaded, contact your doctor. That could mean you’re losing too much fluid too fast.



Matt Gonzales
October 31, 2025 AT 08:20Man, I wish I’d known about urea sooner. My mom was on Natrise for 8 months and her liver enzymes went nuts. We switched her to urea powder mixed in orange juice-she says it tastes like salty candy now, and her sodium’s been stable for 6 months. Cost? $90 a month vs $1,700. Why isn’t this more common in the US? 🤔
Angie Romera
November 2, 2025 AT 02:00So natrise is basically a fancy diuretic with a $2000 price tag and a liver bomb? 😭 I’m not even mad, just disappointed. Like, why do pharma companies make us suffer like this?
Jay Williams
November 3, 2025 AT 19:07Let me offer some perspective: while Natrise has legitimate risks, it remains a critical tool for patients with acute, symptomatic hyponatremia who are not candidates for conservative management. The FDA’s boxed warning is not a ban-it’s a call for vigilance. Monitoring liver enzymes monthly, ensuring adequate hydration, and avoiding CYP3A4 inhibitors mitigates most risk. For patients with SIADH secondary to malignancy, the tradeoff between rapid correction and liver toxicity is often worth it. Alternatives like urea and demeclocycline are valuable, but they lack the speed and predictability of tolvaptan in life-threatening cases. This isn’t about drug preference-it’s about clinical context. Always individualize treatment. The data supports this.
Sarah CaniCore
November 5, 2025 AT 06:53Urea? Really? That’s what you’re recommending? Like, the stuff in fertilizer? 😒 I mean, if you’re gonna go full hippie, at least get the FDA-approved version. This post is just… lazy.
Geoff Colbourne
November 5, 2025 AT 12:58Everyone’s acting like Natrise is the devil, but have you seen the ER stats? People die from hyponatremia because their doctors were too scared to use it. I’ve seen it. My cousin was in a coma from SIADH. They gave him tolvaptan, he woke up in 36 hours. Now he’s on urea because he’s cheap and scared of side effects. But if they’d waited for ‘natural’ fixes, he’d be dead. Stop romanticizing salt tablets.
RaeLynn Sawyer
November 7, 2025 AT 08:11Urea is the real MVP. Natrise is corporate greed in a pill.
Julisa Theodore
November 7, 2025 AT 19:38So we’re all just… floating in a sea of sodium? Like, is this what human biology even is? A broken water balance system waiting for Big Pharma to slap a $1,500 bandaid on it? I mean, why not just drink seawater? 😏
Alice Minium
November 8, 2025 AT 15:28i tried fluid restriction for 3 weeks. i cried every night. my therapist said i was ‘hydrated emotionally but dehydrated physically.’ weird but true.
Richard Poineau
November 9, 2025 AT 09:26You people are all so naive. Urea? Demeclocycline? Those are just bandaids for people who can’t handle responsibility. The real problem? You’re drinking too much water. Stop being so weak. If you can’t control your thirst, maybe you shouldn’t be allowed to drink anything. This isn’t a medical issue-it’s a character flaw.
Keith Terrazas
November 10, 2025 AT 11:49While I appreciate the comprehensive breakdown, I must respectfully submit that the framing of Natrise as a ‘last resort’ is both misleading and statistically unsupported. The literature, particularly the EVEREST and SALT trials, demonstrates that in appropriately selected patients-those with euvolemic hyponatremia and preserved renal function-tolvaptan reduces hospital readmissions by 42% compared to fluid restriction alone. The liver toxicity risk, while real, is mitigated by mandatory monthly LFTs, which are standard of care. To dismiss it as ‘dangerous’ without acknowledging its mortality-reducing benefits is not only irresponsible-it is clinically dangerous. We do not abandon effective therapies because they are expensive or inconvenient. We advocate for better access, not worse outcomes.
Janet Carnell Lorenz
November 11, 2025 AT 13:04My dad switched from Natrise to urea after his liver enzymes spiked. He was so tired of being thirsty all day. Now he just mixes the powder with cranberry juice and calls it a day. He’s been stable for a year. No more midnight bathroom runs. No more $1,500 bills. Just… peace. I wish someone had told us this sooner.
Michael Kerford
November 13, 2025 AT 04:59Why is everyone acting like this is new info? I’ve been on urea since 2020. It’s literally the only reason I’m still alive. Natrise? Nah. I’d rather taste like a salt lick than risk my liver.
Jamie Gassman
November 14, 2025 AT 05:37Let’s be real: the reason there’s no generic tolvaptan isn’t because no one can make it-it’s because the FDA and Big Pharma are in a secret handshake. They want you dependent on the $1,800 pill so you keep coming back. Urea is cheaper, safer, and has been used for 50 years in Europe. Why? Because they don’t have lobbyists here. This isn’t medicine. It’s capitalism with a stethoscope.