CNI Side Effect Risk Calculator
Cyclosporine
First-generation calcineurin inhibitor
Tacrolimus
More potent second-generation option
Your Side Effect Risk Assessment
What Are Calcineurin Inhibitors and Why Are They Used?
Calcineurin inhibitors (CNIs) are powerful drugs that stop your immune system from attacking a transplanted organ. They work by blocking calcineurin, a protein that tells immune cells to become active. Without this signal, T-cells can’t ramp up their attack - which is exactly what you want after a kidney, liver, or heart transplant.
Cyclosporine and tacrolimus are the two main drugs in this class. Cyclosporine has been around since the 1980s. It was the first drug that made long-term organ transplants possible. Tacrolimus came later, in the 1990s, and quickly became more popular because it works better at preventing rejection. Today, about 85% of kidney transplant patients in the U.S. take tacrolimus. Only 10% still use cyclosporine.
But here’s the catch: these drugs don’t just calm your immune system. They also mess with your kidneys, nerves, blood sugar, and more. The goal isn’t just to keep your new organ alive - it’s to keep you healthy while doing it.
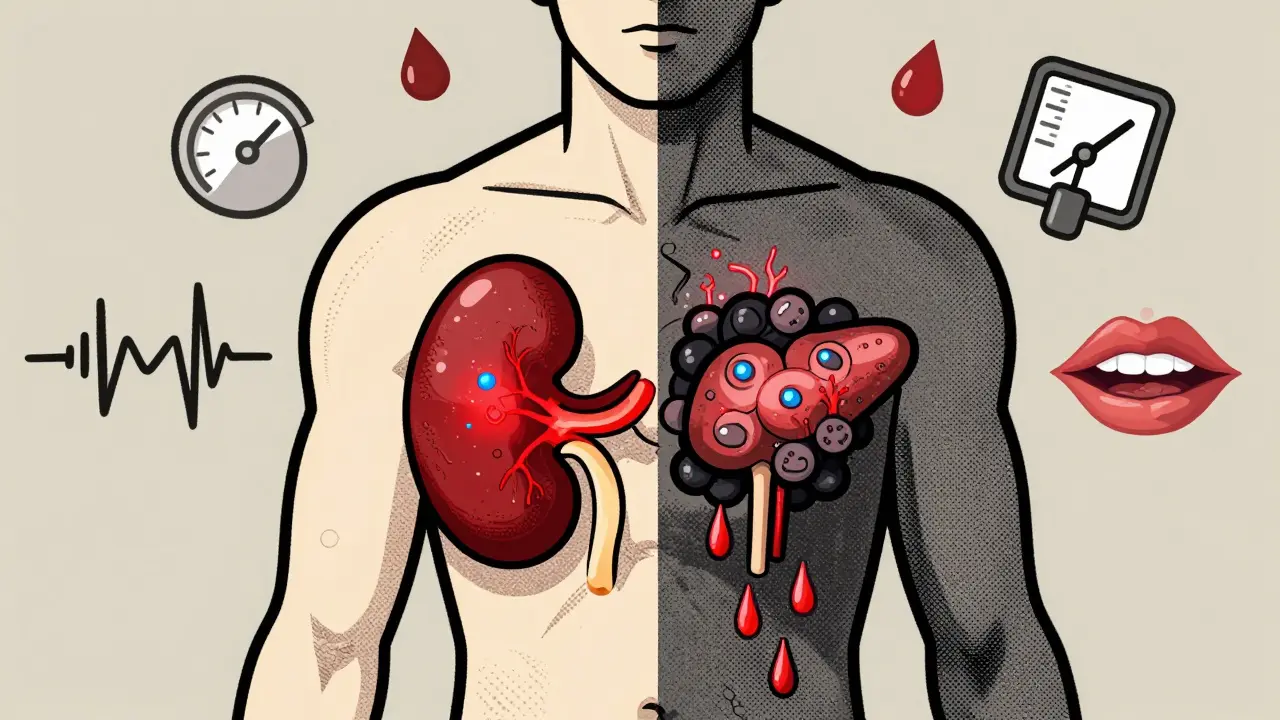
Most Common Side Effects: Kidneys, Blood Pressure, and Electrolytes
Nephrotoxicity - damage to the kidneys - is the biggest problem with both drugs. Up to 75% of patients see their creatinine levels rise within the first few months. That doesn’t always mean permanent damage. Often, it’s just the blood vessels in the kidneys tightening up, which is reversible if caught early.
But for 10-30% of long-term users, the damage becomes permanent. Scar tissue builds up in the kidney tubules. That’s called chronic interstitial fibrosis. A major study from 2009 found that calcineurin inhibitors caused 38% of late kidney graft failures. That’s more than rejection, infection, or high blood pressure combined.
Both drugs also raise blood pressure in 50-70% of patients. That’s partly because they cause your body to hold onto sodium and water. You’ll likely need extra blood pressure meds.
Electrolytes get thrown off too. Magnesium levels drop in 40-60% of users. That can cause muscle cramps, irregular heartbeat, or fatigue. Doctors usually start you on magnesium supplements right away. Potassium goes up too - hyperkalemia affects 20-35% of people. That’s dangerous if left unchecked. Regular blood tests are non-negotiable.
Tacrolimus vs Cyclosporine: The Neurotoxicity Battle
If you’ve ever seen someone with a constant hand tremor after a transplant, it’s probably tacrolimus. Neurotoxicity is much more common with tacrolimus than cyclosporine. Between 30% and 70% of tacrolimus users get tremors. With cyclosporine, it’s only 10-25%.
It’s not just shaking. Headaches, trouble sleeping, confusion, and even seizures can happen. One case study in 2022 described a kidney transplant patient who developed full-blown parkinsonism - slow movement, stiffness, tremors - just two weeks after starting tacrolimus. His symptoms vanished when they switched him to cyclosporine. But then, after eight months on cyclosporine, the tremors came back. That’s how unpredictable this can be.
Doctors now screen for subtle cognitive changes in tacrolimus patients. At UCSF, they do formal memory and attention tests at 3 months. About 15-20% of patients show mild decline. It’s not dementia, but it’s enough to affect daily life - forgetting names, struggling to focus at work, feeling mentally foggy.
The fix? Lowering the dose. Reducing tacrolimus trough levels from 8-10 ng/mL down to 3-5 ng/mL helped 78% of patients stop shaking within four weeks. That’s a huge win. But you can’t just lower it blindly. Too little, and your body starts rejecting the transplant.

Diabetes Risk: Why Tacrolimus Is the Bigger Culprit
New-onset diabetes after transplant (NODAT) is one of the most feared side effects. It’s not just about sugar spikes - it increases heart disease, nerve damage, and kidney problems long-term.
Tacrolimus is far worse here. Between 15% and 30% of people on tacrolimus develop diabetes. With cyclosporine, it’s only 5-15%. Why? Tacrolimus directly damages insulin-producing beta cells in the pancreas. It blocks the calcineurin-NFAT pathway that those cells need to release insulin properly.
A 2021 trial called CIRT-T showed something powerful: if you start an SGLT2 inhibitor (like dapagliflozin) as soon as blood sugar starts creeping up, you cut the risk of full-blown diabetes by 38%. That’s now standard advice in the latest guidelines.
Patients on tacrolimus often need to check their blood sugar daily. Some end up on insulin. Others switch drugs entirely. One patient told me he went from running marathons to needing a cane because of diabetic neuropathy - all tied to his transplant meds.
Cyclosporine’s Hidden Problems: Hair, Gums, and Stomach
Cyclosporine doesn’t hit the nerves or pancreas as hard, but it has its own ugly side effects. Hirsutism - excessive hair growth - happens in 20-30% of users. Women get thick hair on their face, chest, and back. Men get darker, coarser hair in unusual places. It’s not dangerous, but it’s emotionally devastating for many.
Gingival hyperplasia - swollen, overgrown gums - affects 15-25%. Your gums can grow so much they cover your teeth. You need frequent dental cleanings and sometimes surgery. Brushing harder doesn’t help. It’s a direct drug effect.
Stomach issues are milder with cyclosporine. Nausea? 15-25%. Diarrhea? 10-20%. Tacrolimus? 30-45% nausea, 25-40% diarrhea. That’s why some patients switch from tacrolimus to cyclosporine - not for better kidney protection, but because they can’t eat or sleep without constant stomach upset.
How Doctors Manage These Side Effects Today
It’s not about picking the ‘better’ drug. It’s about matching the drug to the patient.
Doctors now use minimum effective dose strategies. Instead of pushing to the highest tolerated level, they aim for the lowest level that still prevents rejection. For tacrolimus, that’s 5-10 ng/mL. For cyclosporine, it’s 100-200 ng/mL. Trough levels are checked weekly when doses change.
Many centers now use CNI-sparing protocols. If you’re low-risk - no prior rejections, good tissue match, no antibodies - you might get a drug like belatacept instead. Belatacept is CNI-free. A 2023 trial showed it gives the same graft survival as tacrolimus but with much better kidney function and fewer metabolic problems.
For patients with severe tremors or diabetes, switching to an mTOR inhibitor like sirolimus is common. It’s not perfect - it can cause mouth sores and high cholesterol - but it doesn’t hurt kidneys or pancreas the same way.
And now, there’s voclosporin. Approved in 2021 for lupus nephritis, it’s a newer CNI with 30% less hypertension than cyclosporine. It’s not yet used in transplants, but trials are underway.

What Patients Are Really Saying
Behind the numbers are real people. On transplant forums, 68% of 1,245 patients on tacrolimus reported moderate to severe side effects. Tremors, sleep loss, and managing diabetes were top complaints.
On Reddit’s r/transplant, cyclosporine users talk about hirsutism constantly. One woman said she stopped wearing tank tops for five years because of facial hair. Another man said his gums grew so much he couldn’t smile in photos.
A 2022 study measured quality of life. People on CNIs scored 15-22 points lower on a 100-point scale than those on CNI-free regimens. That’s like going from feeling fine to feeling constantly unwell.
And here’s the kicker: 78% of patients surveyed by the National Kidney Foundation said they’d switch to a different drug - even if it cost more - if it meant fewer side effects.
What You Can Do: Monitoring, Lifestyle, and Questions to Ask
If you’re on cyclosporine or tacrolimus, here’s what you need to do:
- Get blood tests every week when starting, then monthly once stable - check creatinine, magnesium, potassium, glucose, and drug levels.
- Take magnesium supplements if your doctor recommends them. Don’t skip them.
- Watch for shaking, confusion, or mood changes. Report them immediately.
- Check your blood sugar daily if you’re on tacrolimus, even if you’re not diabetic yet.
- Brush and floss twice a day. See a dentist every 3-4 months.
- Ask your doctor: ‘Is my dose the lowest it can be?’ and ‘Could I try a CNI-sparing regimen?’
These drugs saved your life. But they don’t have to ruin the rest of it. The goal now isn’t just survival - it’s living well.
What’s Next? The Future of Transplant Medications
Researchers are racing to replace CNIs. Belatacept is already proving it can match transplant success without the kidney damage. The NIH-funded CIRT-T2 trial is testing early CNI withdrawal in low-risk patients. Early results show 89% graft survival with 40% fewer side effects.
By 2025, European guidelines want half of all transplant patients off CNIs. The U.S. is catching up. The future isn’t about stronger immunosuppression - it’s about smarter, gentler, personalized treatment.
You don’t have to accept tremors, diabetes, or swollen gums as your new normal. There are options. Ask for them.


Elizabeth Ganak
December 26, 2025 AT 17:57Liz MENDOZA
December 28, 2025 AT 09:28Raushan Richardson
December 29, 2025 AT 18:50dean du plessis
December 30, 2025 AT 11:12Robyn Hays
December 30, 2025 AT 13:47Satyakki Bhattacharjee
January 1, 2026 AT 10:21Kishor Raibole
January 1, 2026 AT 10:36John Barron
January 1, 2026 AT 13:34Jane Lucas
January 3, 2026 AT 07:23Miriam Piro
January 4, 2026 AT 10:30Paula Alencar
January 6, 2026 AT 00:08