Medication Heat Exposure Calculator
Calculate Potency Loss
Enter deployment conditions to see how heat affects medication efficacy.
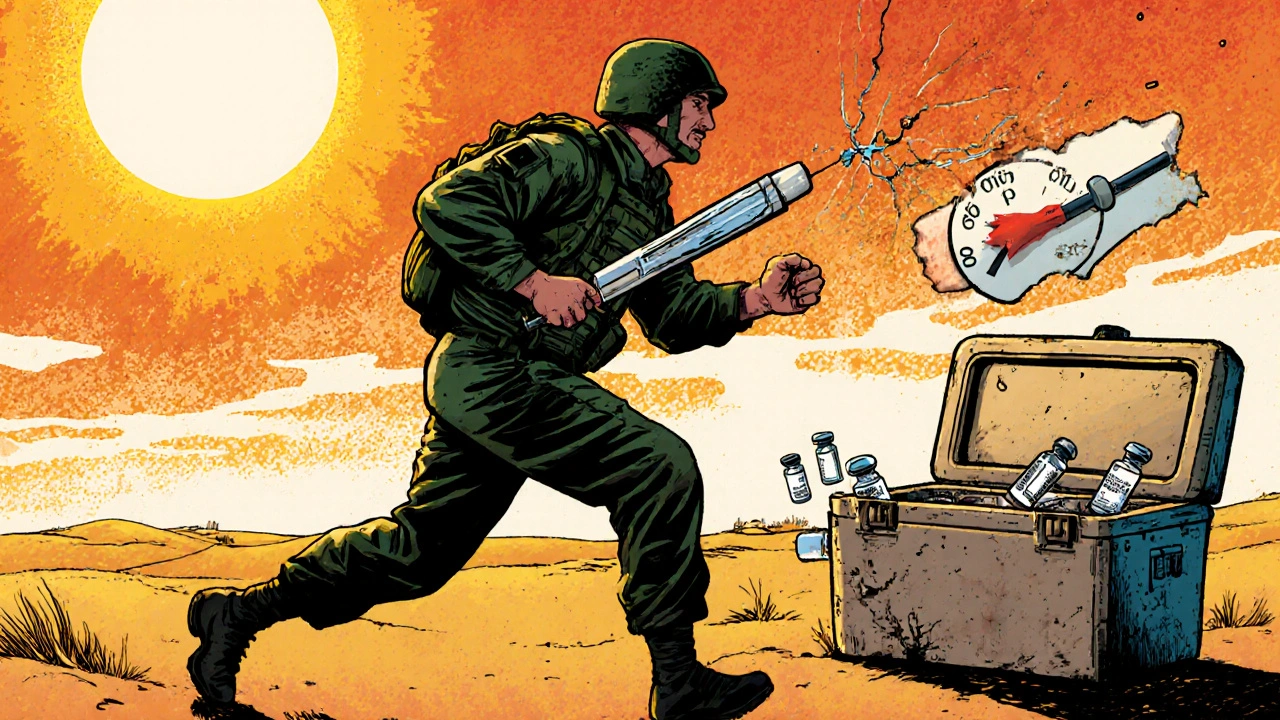
When a soldier needs an epinephrine auto-injector during a heatwave in the Middle East, or a vaccine must stay cold for 72 hours in a desert convoy, the difference between life and death isn’t just about skill-it’s about military medication safety. In civilian pharmacies, refrigerators hum steadily in climate-controlled rooms. In the field, those same medicines are packed into backpacks, left in trucks baking at 50°C (122°F), or stored in tents where the temperature spikes faster than a soldier’s heart rate. The military doesn’t have the luxury of backup power or reliable supply chains. One missed temperature check, one broken cooler, one delayed delivery-and a life-saving drug can become useless.
What Happens When Medicines Get Too Hot?
Vaccines like those for Anthrax, Rabies, and COVID-19 aren’t just pills. They’re complex biological products. Their active ingredients are proteins, viruses, or mRNA strands that break down when exposed to heat. The U.S. Army’s own data shows that some vaccines lose up to 50% of their potency in just 30 minutes when stored above 30°C (86°F). That’s not theoretical. In 2023, units deployed in Iraq and Afghanistan saw 18% of their antibiotics drop below effective levels after being exposed to high heat for more than 48 hours. Antibiotics don’t just stop working-they can become unpredictable, increasing the risk of treatment failure or even antibiotic resistance. Insulin is even more fragile. A soldier with Type 1 diabetes can’t afford a degraded dose. Studies show insulin loses effectiveness rapidly when stored above 30°C, and in extreme heat, the chemical structure changes so much that it no longer binds properly to receptors. Epinephrine auto-injectors, used for anaphylaxis, are another critical concern. While they may still deliver the drug after extreme heat exposure, the buffer solution inside can change pH levels, altering how fast the drug is absorbed. That 15% difference in ionization might mean the difference between a life saved and a life lost.The Cold Chain in Combat Zones
The military calls it the Cold Chain Management (CCM) system. It’s not just about refrigerators-it’s a full logistics pipeline from manufacturer to medic. Every shipment of temperature-sensitive medical products (TSMPs) must be packed with phase-change gel packs and digital temperature loggers like 'Temp-Tale.' These devices record every minute of the journey, proving the meds stayed between 2°C and 8°C. If the logger shows a spike above 8°C, the entire batch is flagged for review. In civilian settings, a brief excursion might be written off. In the military, it’s a mission-critical event. The rules are strict. Every refrigeration unit in a forward medical station must have two temperature monitors: one digital, one manual. Logs must be checked twice a day, every single day. No exceptions. And if the power goes out? The standard operating procedure requires moving all TSMPs to a backup site within 30 minutes. That’s not always possible. In 2023, 37% of refrigeration failures in forward units were caused by generator breakdowns. When that happens, medics scramble-using MRE coolers lined with phase-change materials, wrapping vials in wet cloth to keep them cool through evaporation, even burying insulin in the sand at night to use the earth’s natural cooling.Access Delays in Extreme Heat
It’s not just about storage. It’s about getting the medicine to the person who needs it. In temperate conditions, a medic can administer an IV antibiotic in 12 minutes. In 35°C+ heat, that time jumps to 47 minutes. Why? Because every step takes longer. Gloves sweat and stick. Syringes clog. IV bags fog up. The soldier is dehydrated, shaking, confused. The medic is exhausted, wearing full gear, and under fire. The heat slows everything down-except the clock ticking on the medication’s viability. Personal medications are even harder to manage. Soldiers carry auto-injectors, insulin pens, or seizure meds in their pockets or packs. There’s no climate control. No fridge. Just body heat and desert sun. A 2024 survey of 327 deployed medics found that 83% of medication compromises involved insulin or epinephrine-exactly the drugs that can’t afford to degrade. One medic from Camp Arifjan reported losing six insulin vials in a single week because the unit’s cooler failed and no backup was available.
How the Military Is Fighting Back
The military isn’t just reacting-it’s innovating. In 2022, the Army rolled out mandatory digital temperature logs across all combatant commands, eliminating paper logs entirely. That saved medics 45 minutes a day per unit-time that could be spent on patient care instead of paperwork. The 'Temp-Tale' system reduced medication waste by $2.3 million annually in CENTCOM theaters alone. New tech is coming fast. In March 2025, AI-powered predictive modeling was tested at Fort Bragg. It analyzed weather, transport routes, and equipment history to forecast temperature risks before they happened. The result? A 22% drop in excursions. The Defense Advanced Research Projects Agency (DARPA) is funding a $28 million program called StablePharm, aiming to create antibiotics and vaccines that can survive up to 65°C (149°F) by 2027. Early results show 40% better stability in heat-exposed samples. The goal is simple: make medicines that don’t need refrigeration. If a vaccine can sit in a soldier’s pocket for days in 50°C heat and still work, the entire supply chain changes. No more gel packs. No more generators. No more 30-minute scrambles when the power fails.What’s at Stake
This isn’t about bureaucracy. It’s about readiness. In Operation Inherent Resolve, units with documented temperature excursions during vaccine transport had 12% lower seroconversion rates-meaning fewer soldiers developed immunity. That’s not just a lab number. It’s a unit that can’t deploy because half the troops are vulnerable to disease. A single missed vaccine dose can lead to an outbreak that shuts down an entire base. Climate change is making it worse. Middle Eastern deployment zones saw 23 more days above 40°C in 2024 than in 2020. The RAND Corporation warns that without new heat-stable drugs, medication efficacy could drop by 15-20% by 2030 in high-heat scenarios. That’s not a future problem-it’s a current threat.

Kimberley Chronicle
November 24, 2025 AT 08:48Just read this and my brain is buzzing. The fact that vaccines lose 50% potency in 30 minutes above 30°C is terrifying-this isn’t just logistics, it’s pharmacokinetic warfare. Temp-Tale logs are a start, but we need real-time telemetry with blockchain-backed audit trails. Phase-change materials are clever, but they’re still passive buffers. What if we integrated nanoscale thermal regulators into the vial packaging? DARPA’s StablePharm is promising, but we’re still treating symptoms, not the disease. We need heat-stable formulations designed from the molecular level up-not retrofitted after the fact. The military’s obsession with SOPs is crippling innovation. Medics are improvising with thigh-worn insulin pouches? That’s not a workaround-it’s a systemic failure dressed in duct tape and hope.
Shirou Spade
November 25, 2025 AT 07:36It’s strange how we build empires on the backs of fragile molecules. A strand of mRNA, a protein fold-so delicate, yet they carry the weight of a soldier’s life. We send them into deserts hotter than hell’s kitchen and expect them to behave like lab specimens. Maybe the real question isn’t how to keep medicine cold, but why we keep sending people into places where cold is a luxury. The body adapts. The mind adapts. But biology? Biology doesn’t negotiate. It just breaks.
Lisa Odence
November 27, 2025 AT 03:55OMG this is so important!! 🤯 I’m a clinical pharmacist and I literally cried reading about the insulin vials melting in MRE coolers. 😭 The U.S. Army has spent over $2.3M saving meds via Temp-Tale? That’s a drop in the bucket compared to the cost of failed deployments and antibiotic resistance. 📊 We need mandatory AI-driven predictive modeling at EVERY forward aid station-like, NOW. And DARPA’s StablePharm? GENIUS. 🚀 But why isn’t Congress funding this like it’s a national security emergency? 🇺🇸 We’re talking about life-or-death biochemistry here, not some bureaucratic checkbox! 💉🔥 #MedicineIsWarfare #HeatStableVaccinesNow
Patricia McElhinney
November 28, 2025 AT 09:59This is exactly why I’ve been saying for YEARS that the military is run by overpaid bureaucrats who don’t understand field medicine. 🤦♀️ You think a medic gives a damn about your 40-hour training modules when their cooler just died and they’ve got a diabetic soldier shaking in a 48°C tent? NO. You need to stop the paperwork and give them tools that WORK. And stop using ‘phase-change gel packs’ like they’re magic. They’re not. They’re glorified ice packs that melt faster than a snowman in July. The real solution? Stop using fragile biologics in combat zones. Period. Use synthetic analogs. Use stabilized analogs. Or better yet-DON’T SEND SOLDIERS INTO DESERTS THAT ARE BECOMING UNINHABITABLE. But no, we’d rather spend billions on drones than fix the damn fridge. 🤬
Dolapo Eniola
November 28, 2025 AT 15:54USA thinks it’s the only one with problems? 😂 In Nigeria, we’ve been dealing with heat-degraded meds since the 70s. No Temp-Tale. No AI. No fancy gel packs. We just used the shade, the earth, and our wits. You think your soldiers are suffering? Try being a medic in Kano with 50°C heat, no electricity, and a single fridge that runs on diesel you had to bribe a colonel for. We didn’t wait for DARPA. We made do. Your ‘system’ is broken because you’re too soft to adapt. We didn’t need a $28M program-we needed courage. And you? You need to stop writing essays and start shipping real solutions. 🇳🇬🔥
Agastya Shukla
November 30, 2025 AT 02:28Let me tell you something-this isn’t just about medicine. This is about how we treat the people who keep us safe. That medic in Kuwait carrying insulin on his thigh? That’s not a hack. That’s heroism. That’s the kind of ingenuity that wins wars, not PowerPoint slides from HQ. I’ve seen medics in the field sleep with their coolers because they’re scared to let them out of sight. I’ve seen them cry because they lost a vial and didn’t know if the next one would arrive in time. This isn’t a logistics problem. It’s a moral one. We ask them to risk everything-and then we give them tools that fail because someone thought ‘paper logs are fine.’ We owe them better. Not more rules. Not more training. Just… better gear. And maybe, just maybe, some damn respect.
Patricia McElhinney
December 1, 2025 AT 06:05Wow. You think carrying insulin on your thigh is ‘heroism’? That’s a violation of FDA guidelines, CDC protocols, and every single military medical SOP. It’s not ‘ingenuity’-it’s negligence. You’re romanticizing incompetence. If your meds are that fragile, you shouldn’t be deploying them. Period. The solution isn’t to let medics become amateur pharmacists-it’s to fix the supply chain. And that starts with eliminating all temperature-sensitive biologics from combat zones. Use synthetic alternatives. Use oral analogs. Use stable formulations. Stop pretending that duct-taping a cooler to a soldier’s leg is a viable strategy. It’s not. It’s a disaster waiting to happen. And if you’re celebrating it, you’re part of the problem.