When working with ice therapy, the application of cold to body tissues to reduce pain, swelling, and inflammation. Also known as cold therapy, it is a cornerstone of many treatment plans. A related concept is cryotherapy, a broader term that covers whole‑body and localized cold treatments. Another key player is pain relief, the primary goal for most people using ice.
Ice therapy reduces inflammation by narrowing blood vessels, which limits fluid buildup in injured tissues. This physiological response is called vasoconstriction, and it helps keep swelling in check. Because swelling often fuels pain, controlling it directly supports inflammation reduction. The colder the pack, the more pronounced the effect, but timing matters: a typical cycle is 15‑20 minutes on, followed by at least 40 minutes off. This cycle prevents skin damage while keeping the therapeutic chill active.
Where does ice therapy shine most? In the world of sports injuries, athletes rely on rapid swelling control to get back on the field. From sprained ankles to strained muscles, a cold compress can cut recovery time dramatically. It’s also a staple after surgeries, where surgeons aim to limit post‑operative bruising and discomfort. Even chronic conditions like arthritis benefit from occasional cold application, as the cooling effect eases joint stiffness without the side effects of medication.
To get the most out of ice therapy, follow three simple rules. First, always wrap the ice pack in a thin towel—direct skin contact can cause frostbite. Second, monitor the clock; exceed 20 minutes and you risk numbing nerves, which slows healing. Third, combine cold with elevation when possible; lifting the injured limb above heart level further drains fluid. These steps turn a simple cold compress into a powerful recovery tool.
Beyond the basics, consider the type of cold source you use. Traditional gel packs, frozen peas, or even a bag of ice cubes work, but each has a different heat‑retention profile. Gel packs stay cold longer, making them ideal for longer sessions, while frozen peas conform to body contours, perfect for joint areas. Experiment to see which suits your routine best.
Remember, ice therapy isn’t a one‑size‑fits‑all solution. People with certain circulatory disorders, diabetes, or hypersensitivity should consult a healthcare professional before starting. When used correctly, though, the benefits – faster swelling control, reduced pain, and quicker return to activity – are hard to beat.
Below you’ll find a curated set of articles that dive deeper into specific drugs, conditions, and treatment comparisons that intersect with ice therapy. From detailed drug histories to side‑effect breakdowns, these posts give you the broader medical context you need to make informed decisions about your recovery plan.
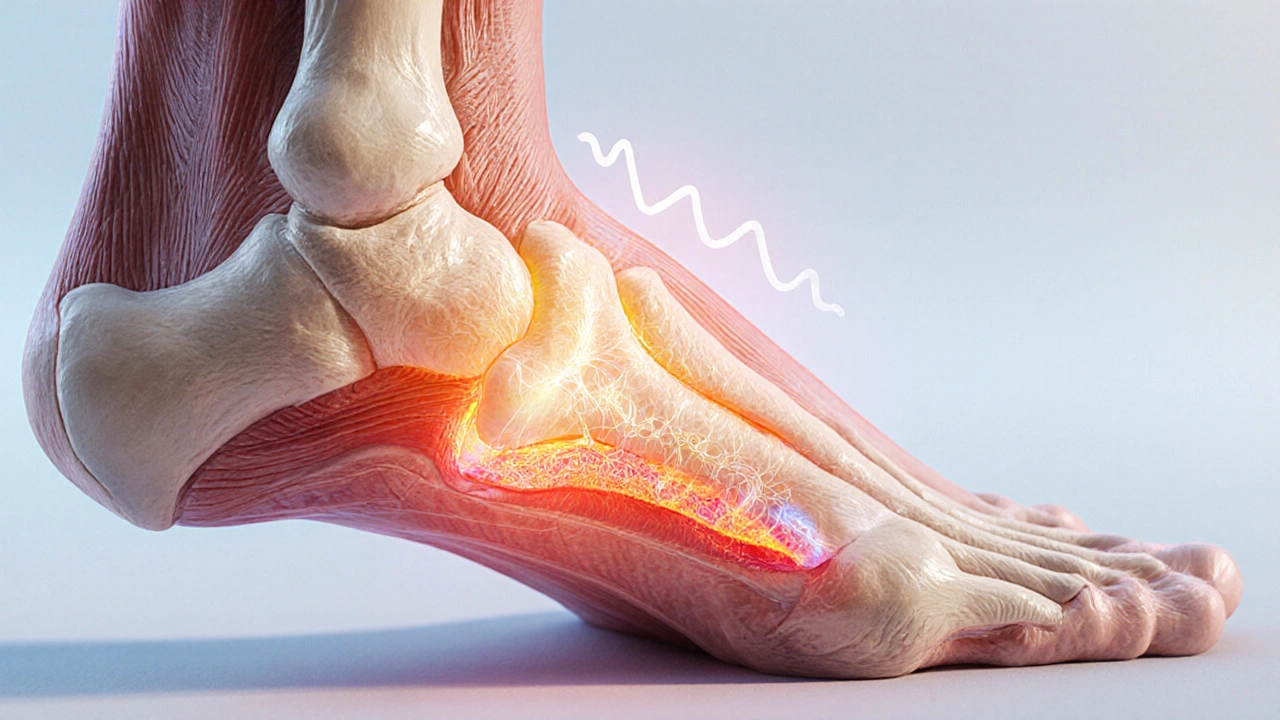
Discover how to soothe tendonitis pain naturally with ice, heat, stretches, strengthening exercises, and anti‑inflammatory herbs for lasting relief.

Finding the right online pharmacy can be vital when looking for affordable medication. Whether you're interested in more international options or simpler ordering processes, there are several alternatives to Canada Drugs Direct that may suit your needs better. This article explores these options, covering each one’s strengths and weaknesses, to help you make an informed choice.

The best time to take statins isn't about night or morning-it's about consistency. Learn how statin timing affects side effects and cholesterol lowering, and why adherence beats clock time.

Dizziness after surgery can be a common yet disorienting experience. This piece explores practical ways to manage dizziness effectively, delving into causes and offering helpful tips for recovery. Understanding how to navigate these post-surgery effects is key to a smoother healing process. Learn what to expect and how to ease this sensation in everyday life.

Trace the journey of HIV from its 1980s discovery to today’s advanced antiretroviral treatments, highlighting key milestones, scientists, and breakthroughs.
Compare Vidalista Professional with Cialis and other tadalafil generics to find the safest, most cost-effective option for treating erectile dysfunction. Learn what really matters-active ingredients, safety, and where to buy.