Living with bronchiectasis means dealing with a cough that won’t quit - one that brings up thick, foul-smelling mucus every day, often in large amounts. It’s not just a bad cold that won’t go away. It’s a lifelong condition where the airways in your lungs have become permanently widened and damaged, making it hard to clear mucus. That trapped mucus becomes a breeding ground for bacteria, leading to frequent infections, more inflammation, and further damage. The cycle is brutal: mucus builds up, infection follows, lungs get worse, and breathing gets harder. But here’s the good news: bronchiectasis isn’t curable, but it’s manageable. With the right daily habits, you can break that cycle, reduce hospital visits, and live better.
What Bronchiectasis Really Feels Like
Most people don’t realize how specific the symptoms are. It’s not just any cough. It’s a daily productive cough that produces at least 30 milliliters of sputum - that’s about two tablespoons - often yellow or green, sometimes with a bad odor. Many patients describe it as a constant wet, gurgling feeling in the chest, even when they’re not sick. Fatigue is common. Shortness of breath during simple tasks like walking up stairs or carrying groceries becomes normal. Some notice their fingers or nails changing shape over time - a sign called clubbing, caused by low oxygen levels in the blood. The real turning point for most is when they finally get a CT scan. That’s the gold standard for diagnosis. On the scan, the bronchial tubes look like thickened, swollen pipes, often wider than the nearby blood vessels. The ratio is clear: if the bronchial artery is more than 1.5 times the size of the pulmonary artery next to it, it’s bronchiectasis. This isn’t something you can miss on a good scan. Yet, many people go years undiagnosed because doctors mistake it for asthma or chronic bronchitis.Why Airway Clearance Isn’t Optional - It’s Essential
The single most important thing you can do for bronchiectasis is clear your airways every single day. No exceptions. Research from the American Thoracic Society shows that patients who skip daily clearance have their lung function decline 45 milliliters per year - nearly double the rate of those who stick to it. That’s not a small difference. That’s the difference between staying independent and needing oxygen therapy within five years. There are several proven techniques. The most common is the Active Cycle of Breathing Techniques (ACBT). It’s a three-step process: breathing control, deep breathing to loosen mucus, then huff coughing to move it out. Huff coughing is different from regular coughing. You take a medium or deep breath, hold it briefly, then exhale forcefully through an open mouth - like you’re trying to fog up a mirror. You do it in bursts, not one big cough. It’s less tiring and more effective. Another option is using a handheld PEP device - like the Aerobika®. You breathe in through a mask, then exhale against resistance. That pressure helps open blocked airways and moves mucus upward. Studies show it clears 35% more mucus than traditional chest tapping, and it costs under $200. Compare that to an oscillating vest that costs $6,000. For most people, the PEP device is the smart choice. Nebulized hypertonic saline - a saltwater mist at 7% concentration - is another powerful tool. It draws water into the mucus, thinning it so it’s easier to cough out. When combined with dornase alfa, it works even better. Many patients report feeling lighter in the chest within minutes after using it. The key? Do it twice a day, 15 to 20 minutes each time. It’s not a suggestion. It’s medical treatment. Dr. Shivani Gupta at Penn Medicine puts it bluntly: “Daily airway clearance isn’t optional - it’s as essential as taking antibiotics.”Antibiotics: When and How to Use Them
Antibiotics are a necessary part of managing bronchiectasis, but they’re not a cure. They’re a tool to stop infections before they wreck your lungs. The goal isn’t to kill every germ - it’s to prevent the big, damaging ones from taking over. For frequent infections - three or more flare-ups a year - long-term, low-dose antibiotics are often prescribed. Azithromycin, taken three times a week (usually 250-500mg), has been shown in clinical trials to cut exacerbations by 32%. It’s not just killing bacteria; it’s also reducing inflammation in the airways. That’s why it works better than just treating flare-ups. For patients with Pseudomonas aeruginosa - a tough, common bug in bronchiectasis - inhaled antibiotics like tobramycin are used. These are delivered directly to the lungs via nebulizer, so you get high doses where you need them, with fewer side effects than pills. Studies show they reduce colonization by 56%. But here’s the danger: overusing antibiotics without clearing mucus first leads to resistance. Dr. Michael J. Rock at the University of Wisconsin warns that 38% of patients develop antibiotic-resistant bacteria within five years of chronic use. That’s why you never start antibiotics unless you have signs of an active infection - increased mucus, darker color, fever, or worsening breathlessness. Always finish the full course. Never save pills for later. And never take them without a doctor’s guidance. The NHS and American Thoracic Society both stress: intermittent use during flare-ups alone increases the risk of permanent lung damage by 2.3 times.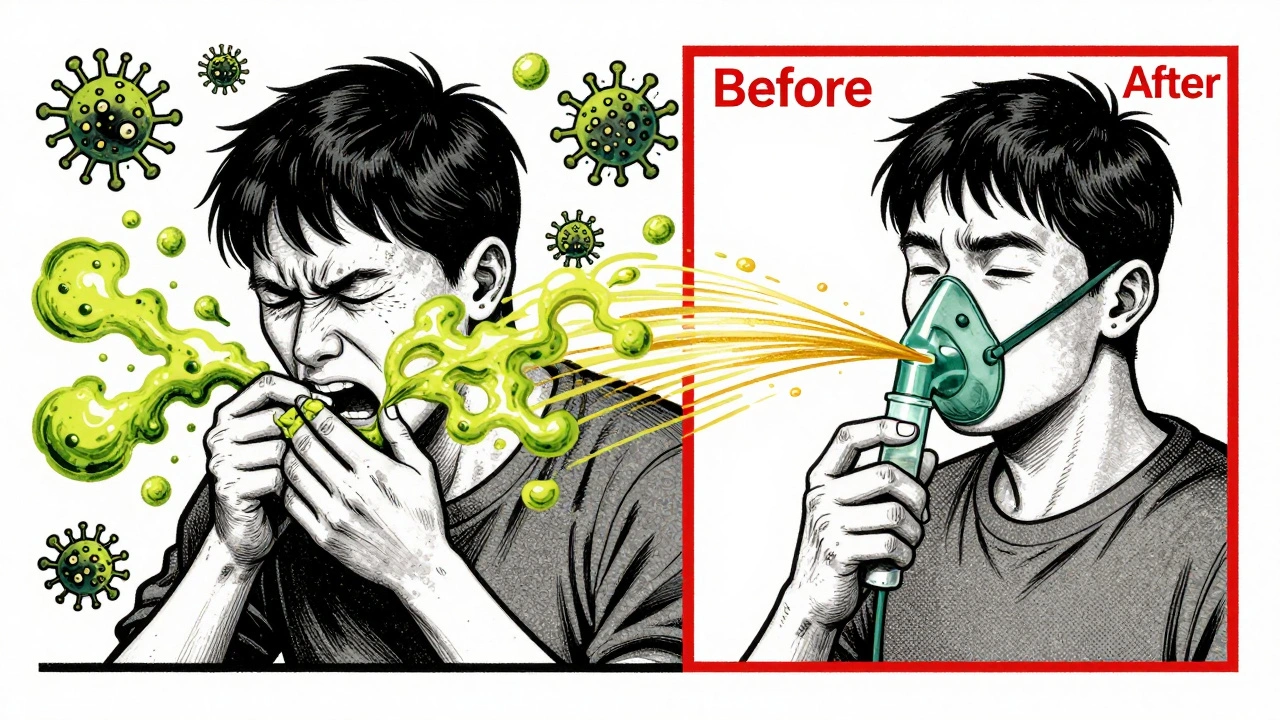
What Doesn’t Work - And Why
Some treatments get a lot of attention but offer little real benefit. Bronchodilators - inhalers meant to open airways - help only 12% of people when used alone. But when combined with airway clearance, that jumps to 28%. So don’t skip the clearing just because you’re using an inhaler. Cough suppressants are a trap. They might make you feel less coughy, but they trap mucus inside your lungs. That’s like putting a lid on a boiling pot - it only makes things worse. Never use them unless you have a dry, hacking cough from something else - like a virus. Steroid inhalers are often prescribed for asthma or COPD, but they’re not recommended for most bronchiectasis patients. They don’t help clear mucus and can increase infection risk. Only use them if you have a confirmed overlap with asthma. And while surgery can help in rare cases - like removing one damaged lobe of the lung - it’s not a first-line treatment. Only about 5% of patients ever need it, and only when the damage is localized and other treatments have failed.Real Life: What Patients Actually Do
On patient forums and support groups, the same patterns keep coming up. Of the 1,243 people on the American Lung Association’s forum, 78% say huff coughing gives them immediate relief during flare-ups. Sixty-three percent say learning the techniques was frustrating at first - but worth it after 6 to 8 weeks. The biggest complaint? Time. Forty-two percent of NHS users say they struggle to fit 20 minutes of daily clearance into their lives - especially if they work long hours, care for kids, or have physical jobs. That’s why simplicity matters. If you can’t do ACBT, use a PEP device. If you can’t do two sessions, do one. Better to do less consistently than to do a lot and quit. One patient in a 2022 American Lung Association spotlight went from nine hospitalizations a year to just one after sticking with daily hypertonic saline and ACBT. That’s not a miracle. That’s discipline. Another common issue? Insurance. Many PEP devices cost $150-$200. Medicare and private insurers often cover them, but only if you have documentation showing you’ve been trained and need them. Ask your respiratory therapist to help you with the paperwork.What’s New and What’s Coming
The field is moving fast. In 2023, the FDA approved gallium maltolate, an inhaled treatment for stubborn Pseudomonas infections. Early trials showed a 42% drop in flare-ups. That’s huge for patients who’ve run out of antibiotic options. Researchers are also looking at the lung microbiome - the collection of bacteria living in your airways. A trial in Scotland is testing inhaled bacteriophages (viruses that target specific bacteria) to wipe out resistant bugs. Early results show 68% success in clearing Pseudomonas without antibiotics. Genetic testing is becoming more common too. The Bronchiectasis Research Registry, launched in 2022, has already found markers that predict who’s likely to decline quickly. By 2025, doctors may be able to tailor treatments based on your genes - not just your symptoms. But the biggest gap isn’t science - it’s access. Medicaid patients have over three times more flare-ups than those with private insurance. Why? They’re less likely to see a respiratory therapist, get trained in clearance techniques, or afford devices. That’s a systemic failure, not a medical one.
How to Get Started
If you’ve just been diagnosed, here’s your roadmap:- Get a high-resolution CT scan to confirm the diagnosis and map the damage.
- Ask for a referral to a respiratory therapist. They’ll teach you how to clear your airways - properly.
- Start daily airway clearance. Pick one method: ACBT, PEP device, or nebulized saline. Stick with it.
- Keep a symptom journal. Note mucus color, volume, cough frequency, and breathing changes. This helps your doctor decide when you need antibiotics.
- Drink at least 2 liters of water a day. Hydration thins mucus. It’s simple, free, and critical.
- Get your flu and pneumonia vaccines every year. Infections are your biggest threat.
- Ask about long-term azithromycin if you’ve had three or more flare-ups in a year.
Frequently Asked Questions
Can bronchiectasis be cured?
No, bronchiectasis cannot be cured because the damage to the airways is permanent. But it can be managed effectively. With daily airway clearance, appropriate antibiotics, and lifestyle changes, most people can slow or stop disease progression, reduce flare-ups, and live full, active lives.
How do I know if I’m clearing my mucus properly?
You should feel a difference - lighter chest, less congestion, and more mucus coming up after your routine. Your respiratory therapist can observe your technique and give feedback. If you’re coughing hard but not producing more sputum, you’re likely not using the right method. Huff coughing should feel like you’re pushing mucus out with controlled breaths, not just choking on it.
Do I need to take antibiotics all the time?
No. Long-term antibiotics like azithromycin are only for people with frequent flare-ups - typically three or more per year. If you’re stable and not getting sick often, you won’t need them. Taking antibiotics unnecessarily increases the risk of resistant infections. Always follow your doctor’s guidance based on your history, not someone else’s.
Why is my sputum green or yellow?
Green or yellow mucus means your immune system is fighting an infection. White blood cells called neutrophils, which are part of your body’s defense, release enzymes that turn mucus that color. It doesn’t always mean you need antibiotics - but if it’s new, thick, or accompanied by fever or worsening breathlessness, it’s a sign to contact your doctor.
Can I exercise with bronchiectasis?
Yes - and you should. Exercise helps strengthen your breathing muscles and improves mucus clearance naturally. Walking, swimming, and cycling are great. Don’t wait until you feel better to start. Even light activity every day helps maintain lung function and reduces flare-up risk. Talk to your therapist about safe routines.
What should I do during a flare-up?
Increase your airway clearance to twice daily. Drink more fluids. Use your prescribed rescue antibiotics if you have a plan from your doctor. Watch for signs of worsening: fever, more mucus, darker color, or trouble breathing. If symptoms don’t improve in 48 hours, call your provider. Don’t wait until you’re in the ER.



Constantine Vigderman
December 13, 2025 AT 21:42Cole Newman
December 15, 2025 AT 05:12Casey Mellish
December 15, 2025 AT 06:05Tyrone Marshall
December 16, 2025 AT 12:49Emily Haworth
December 17, 2025 AT 20:59Tom Zerkoff
December 19, 2025 AT 06:41Yatendra S
December 19, 2025 AT 14:22Webster Bull
December 20, 2025 AT 04:09Scott Butler
December 21, 2025 AT 11:47