When you take more than one medication, your body doesn’t treat them like separate guests—it treats them like roommates sharing the same space. Pharmacokinetic interactions, the way drugs change how your body absorbs, moves, breaks down, or removes them. Also known as drug-drug interactions, they happen before the drug even reaches its target. This isn’t about side effects you feel—it’s about whether your body can even use the drug the way it’s supposed to. For example, if you’re taking ramipril, a blood pressure medication and suddenly start eating a lot of salt, that interaction changes how well ramipril works. Or if you take calcium supplements, often used for bone health at the same time as bisphosphonates, drugs for osteoporosis, the calcium can block absorption so neither works right. These aren’t rare mistakes—they’re everyday risks.
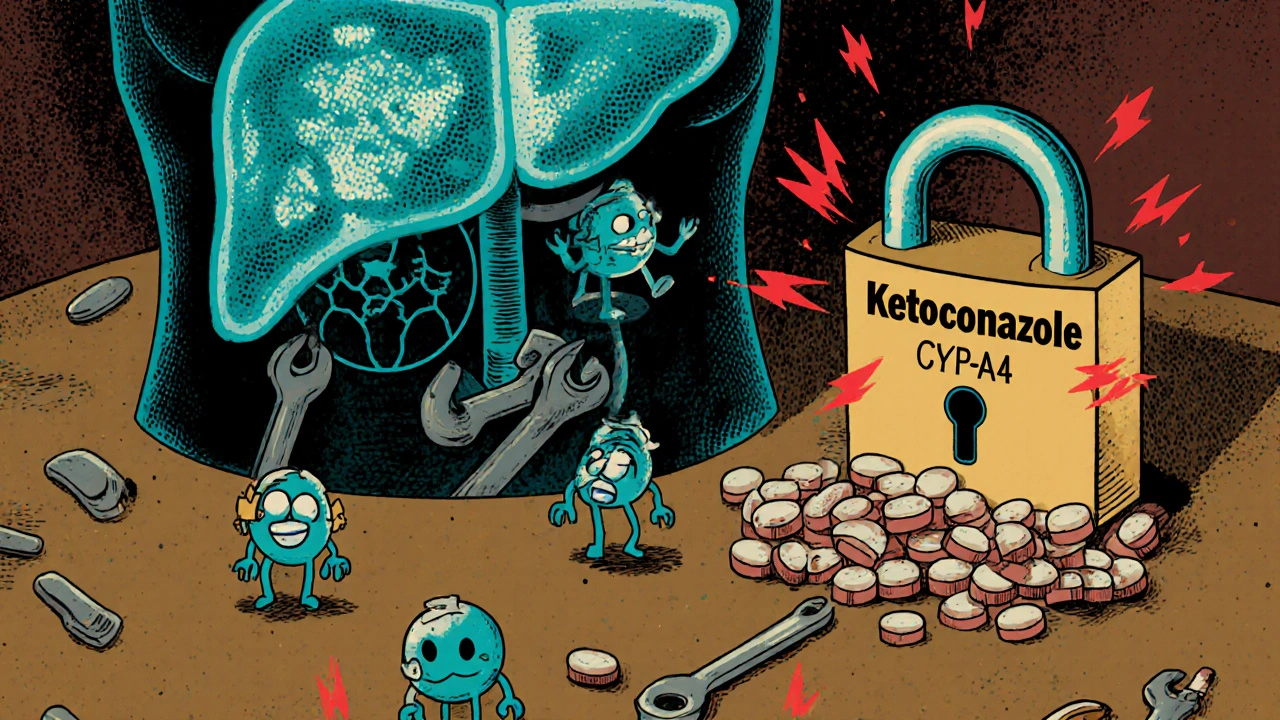
Pharmacokinetic interactions fall into four main buckets: absorption, distribution, metabolism, and elimination. Absorption problems happen when one drug stops another from entering your bloodstream—like how antacids can make your antibiotic useless. Distribution issues occur when drugs compete for protein binding sites in your blood, pushing one into overdrive. But the biggest troublemaker? Metabolism. Your liver uses enzymes—mostly CYP3A4 and CYP2D6—to break down drugs. If one drug slows down those enzymes (like grapefruit juice with statins), others build up to dangerous levels. If another drug speeds them up (like St. John’s wort with birth control), the drug gets cleared too fast and stops working. Then there’s elimination—kidneys flushing out drugs. Some antibiotics can mess with how your kidneys handle other meds, leading to kidney stress or toxicity.
These aren’t just theory. Look at the posts here: people are asking how to time calcium and bisphosphonates, why salt matters with ramipril, and how to avoid liver damage from Natrise. They’re all dealing with the same hidden layer—the body’s internal chemistry. You might think you’re following your doctor’s advice, but if you’re taking five pills a day, some of them are silently working against each other. That’s why a checklist for safe storage isn’t enough—you need to know how your meds interact inside you. The articles below cover real cases: how sedating antihistamines raise fall risk not just from drowsiness, but from how they’re processed with other drugs. How cabergoline’s effects change when mixed with blood pressure meds. How to avoid eye damage from ethambutol because of liver metabolism issues. You won’t find this in the pamphlet that comes with your prescription. You’ll find it here—in plain language, real examples, and practical steps to protect yourself.
Drug-drug interactions can cause serious harm when medications clash in your body. Learn how liver enzymes, transporters, and genetics affect drug safety, and what you can do to avoid dangerous combinations.

A detailed look at Chloramphenicol, its clinical uses, safety concerns, and how it stacks up against common alternatives such as Azithromycin, Ciprofloxacin, and Doxycycline.

Explore how self‑driving cars could reshape traffic jams, the tech behind them, policy levers, real‑world pilots, and what it means for commuters and cities.

Explore how genetics, therapeutic monitoring, and new delivery methods can personalize ethambutol therapy, reduce eye toxicity, and boost TB treatment success.

Explore how support groups improve life for those with partial onset seizures, covering benefits, types, finding options, and tips for active participation.

Over half of patients with chronic conditions skip or forget their medications due to cost, confusion, complex schedules, and fear of side effects. Understanding these barriers is the first step to better health outcomes.