Drug Interaction Checker
Check for Interactions
Every year, thousands of people end up in hospitals not because their illness got worse, but because two medicines they were taking clashed in ways no one expected. One drug might make another too strong-leading to dangerous side effects-or too weak-letting the condition slip out of control. These are drug-drug interactions, and they’re not rare. They’re common, complex, and often preventable.
What Exactly Is a Drug-Drug Interaction?
A drug-drug interaction (DDI) happens when one medication changes how another medication works in your body. It’s not just about pills mixing in a bottle. It’s about what happens inside you-how your liver processes them, how your kidneys flush them out, or how they affect your heart rhythm. There are two main types: pharmacokinetic and pharmacodynamic.Pharmacokinetic interactions are about what your body does to the drug. This includes absorption, distribution, metabolism, and excretion. For example, if you take a drug that slows down your liver’s ability to break down another drug, that second drug can build up to toxic levels. On the flip side, if a drug speeds up metabolism, the other drug might get cleared too fast and stop working.
Pharmacodynamic interactions are about what the drugs do to your body together. Two drugs might target the same system and amplify each other-like two blood thinners making you bleed more. Or they might cancel each other out-like a stimulant and a sedative fighting over your nervous system.
How Your Liver Becomes the Battleground: CYP450 Enzymes
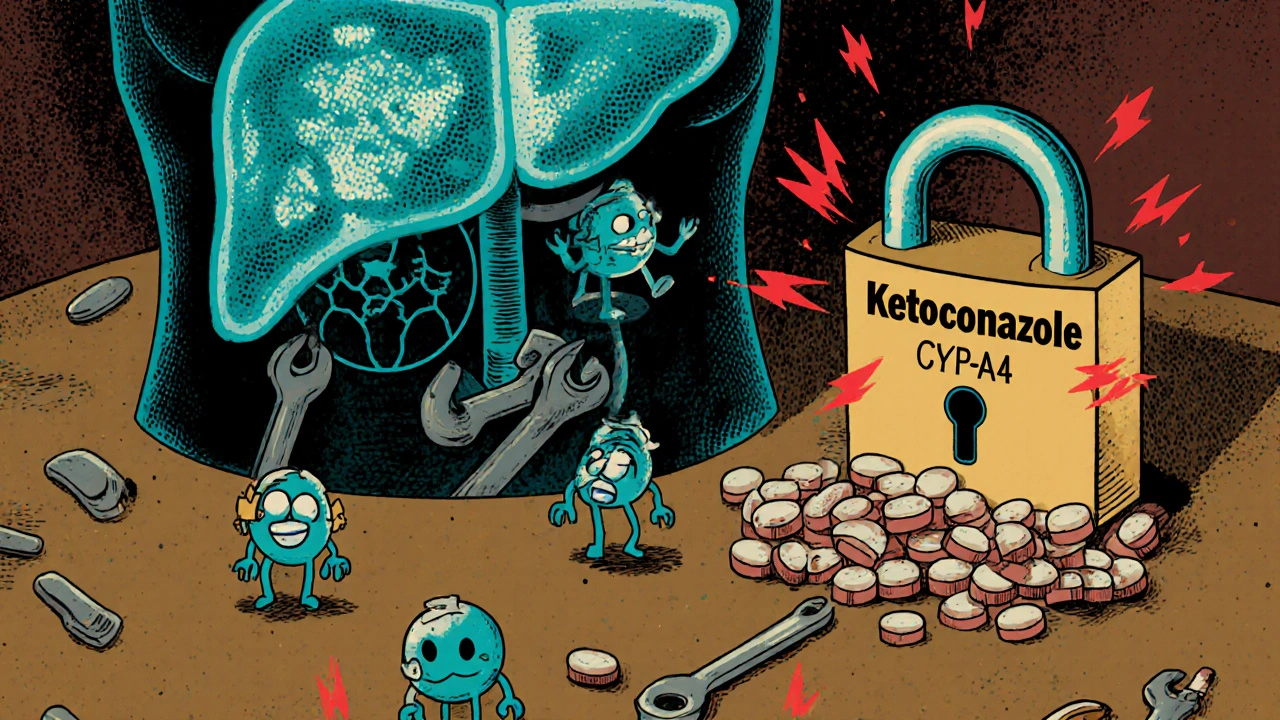
The most common cause of pharmacokinetic interactions involves a family of liver enzymes called cytochrome P450 (CYP450). These enzymes break down about 70-80% of all prescription drugs. Among them, CYP3A4 is the biggest player-it handles roughly half of all medications you take.Some drugs act as inhibitors-they block CYP3A4 like putting a lock on a factory. Ketoconazole, for example, is a strong inhibitor. If you take it with simvastatin (a cholesterol drug), simvastatin can’t break down properly. Its levels can spike 10 to 20 times higher than normal. That’s not just a bump-it’s a direct path to rhabdomyolysis, a condition where muscle tissue breaks down and can damage your kidneys.
Other drugs are inducers. They tell your liver to build more CYP3A4 enzymes, like turning up the factory’s production line. St. John’s Wort, a popular herbal supplement, is one of the strongest inducers. It can slash the levels of drugs like cyclosporine (used after organ transplants) by 50-60%. That means your body might reject the new organ because the drug isn’t working anymore.
These effects are ranked by strength: strong (5-fold or greater change), moderate (2-5-fold), and weak (less than 2-fold). The FDA uses these categories to guide prescribing. But even weak interactions can matter if you’re taking a drug with a narrow therapeutic window-like warfarin, where a tiny change in blood level can mean the difference between clotting and bleeding.
Transporters: The Hidden Gatekeepers
It’s not just the liver. Your cells have tiny gates called transporters that control what gets in and out. One of the most important is P-glycoprotein (P-gp). It’s like a bouncer at the blood-brain barrier or the gut lining, deciding which drugs get through.Verapamil, a heart medication, blocks P-gp. When taken with digoxin-a drug used for heart rhythm problems-it stops digoxin from being pumped out of your cells. Digoxin builds up, and your heart can go into dangerous rhythms. Studies show digoxin levels can jump by 50-100% with this combo.
Another key transporter is OATP1B1, found in the liver. It brings statins into liver cells so they can do their job. If you take it with gemfibrozil (a lipid-lowering drug), OATP1B1 gets blocked. Statins flood into your muscles instead of your liver. That’s why some statin-fibrate combos are now avoided entirely.

When Drugs Talk to Each Other: Pharmacodynamic Clashes
Sometimes, drugs don’t need to change each other’s levels to cause trouble. They just need to act on the same system.Take QT prolongation-the lengthening of the heart’s electrical cycle. Fluoroquinolone antibiotics like levofloxacin and macrolides like erythromycin both do this on their own. Together? The risk of a deadly arrhythmia called torsades de pointes goes up by 5.7 times. This isn’t theoretical. It’s been documented in real patients, and it’s why doctors avoid this combo unless there’s no other option.
Another classic: ACE inhibitors (like lisinopril) plus potassium-sparing diuretics (like amiloride). Both raise potassium. Together, they can push serum potassium up by 1.0-1.5 mmol/L. That’s enough to stop your heart. Elderly patients on multiple medications are especially at risk.
Even something as simple as combining two NSAIDs (like ibuprofen and naproxen) with warfarin can triple your bleeding risk. The NSAIDs thin the stomach lining, and warfarin thins the blood. Together, they’re a recipe for internal bleeding.
Genetics Play a Role-More Than You Think
Not everyone reacts the same way to the same drug combo. Why? Because your genes decide how fast your enzymes work.CYP2D6 is a great example. Some people are “poor metabolizers”-they have a genetic variant that makes this enzyme nearly inactive. Others are “ultrarapid metabolizers,” with extra copies of the gene. Codeine, a common painkiller, needs CYP2D6 to turn into morphine. In poor metabolizers, it doesn’t work. In ultrarapid metabolizers, it turns into too much morphine too fast-especially dangerous if they’re also taking a CYP3A4 inhibitor like clarithromycin.
The Clinical Pharmacogenetics Implementation Consortium (CPIC) has published 22 guidelines for this exact reason. They tell doctors: if you’re prescribing codeine to someone with this genetic profile, don’t. Use something else.
Why This Matters in Real Life
DDIs aren’t just lab curiosities. They cost money. A 2019 study estimated preventable drug interactions cost the U.S. healthcare system $1.3 billion a year-mostly from hospital stays due to bleeding or muscle damage.In the elderly, DDIs cause 3-5% of all hospital admissions. The Beers Criteria, updated in 2019, lists 30 high-risk combinations for people over 65. One of the most dangerous? NSAIDs with anticoagulants. Another? Benzodiazepines with opioids. Both can cause falls, confusion, and death.
Community pharmacists catch a lot of these. One 2021 study found pharmacist-led reviews reduced serious DDIs by 37% in over 12,000 patients. They spot the hidden risks: a patient on warfarin taking a new OTC cold medicine with pseudoephedrine. Or someone on antidepressants starting St. John’s Wort without telling their doctor.

Technology Can Help-But It’s Flawed
Most hospitals and pharmacies use electronic systems that warn about DDIs. But here’s the problem: 80-90% of those alerts are false. Too many warnings mean doctors ignore them. Studies show clinicians override 49-96% of alerts, a phenomenon called “alert fatigue.”Newer systems are smarter. Epic’s “Suggestive Warnings” feature, rolled out in 2021, doesn’t just flag every combo. It looks at the patient’s history, age, kidney function, and other meds. In one trial, it cut high-severity DDIs by 22% across 4.7 million patient encounters.
AI is also stepping in. A 2021 study trained a machine learning model on 89 million electronic health records. It predicted DDIs with 94.8% accuracy-far better than old rule-based systems. The future? Personalized alerts based on your genes, your liver function, your other meds, and even your diet.
What You Can Do
You don’t need to be a doctor to protect yourself. Here’s what works:- Keep a list of every medication you take-prescription, OTC, supplements, herbal products. Bring it to every appointment.
- Ask your pharmacist: “Could any of these interact?” Don’t assume they know. Pharmacists are trained for this.
- Don’t start a new supplement without checking. St. John’s Wort, goldenseal, and grapefruit juice are notorious.
- If you’re on warfarin, keep your vitamin K intake steady. Spinach one day, salad the next? Your INR will swing.
- Report side effects. If you feel weird after starting a new drug, tell your provider. That data helps others.
The Future Is Personalized
The next big shift isn’t just about avoiding bad combos. It’s about predicting the right ones for you. Pharmacogenomics-testing your genes before prescribing-is becoming more common. Hospitals in the UK and U.S. are starting to test for CYP2D6, CYP2C19, and SLCO1B1 variants before giving certain drugs.Research is also looking at the gut microbiome. Bacteria in your intestines can break down drugs before they’re absorbed. One study found that certain gut bugs can deactivate digoxin-meaning two people taking the same dose might have totally different blood levels.
Regulators are catching up too. The FDA now requires drug makers to test for interactions with herbal products and complex regimens of three or more drugs. That’s because most older adults take five or more medications. It’s not an exception-it’s the norm.
Drug interactions aren’t going away. But with better science, smarter tools, and more awareness, we’re getting better at stopping them before they hurt someone.
What are the most dangerous drug-drug interactions?
Some of the most dangerous combinations include warfarin with NSAIDs (triple the bleeding risk), simvastatin with ketoconazole (10-20x increase in muscle toxicity risk), and fluoroquinolones with macrolides (5.7x higher risk of fatal heart rhythm). Also, ACE inhibitors with potassium-sparing diuretics can cause life-threatening hyperkalemia. These are not rare-each has caused real patient deaths.
Can over-the-counter drugs cause dangerous interactions?
Yes. Common OTC products like ibuprofen, pseudoephedrine, and even antacids can interfere with prescription drugs. Ibuprofen can reduce warfarin’s effectiveness or increase bleeding. Pseudoephedrine can raise blood pressure in people on beta-blockers. Antacids can block absorption of antibiotics like ciprofloxacin. Always check with a pharmacist before taking OTC meds with prescriptions.
Does grapefruit juice really interact with medications?
Absolutely. Grapefruit juice blocks CYP3A4 in the gut, which can cause drugs like simvastatin, atorvastatin, and felodipine to build up to toxic levels. Even one glass can have effects lasting over 24 hours. The FDA lists over 85 drugs that interact with grapefruit. If you’re on any statin, blood pressure med, or immunosuppressant, avoid it.
Why do some drug interactions take days to show up?
Because some interactions aren’t immediate. Inducers like St. John’s Wort take days to ramp up enzyme production. Inhibitors like clarithromycin can cause delayed effects if they’re metabolized slowly themselves. Also, some drugs accumulate over time-like digoxin. The full effect of an interaction may not show until after several doses.
Are herbal supplements safer than prescription drugs?
No. Many people assume herbal products are harmless, but they’re not regulated like drugs. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and HIV meds. Goldenseal inhibits CYP3A4 and P-gp. Kava can damage the liver when combined with alcohol or acetaminophen. Always disclose herbal use to your doctor.
How do I know if a new medication is safe with my current ones?
Ask your pharmacist. They have access to real-time databases like the Liverpool HIV-Drug Interactions Checker or Micromedex. If you’re on more than five medications, request a full medication review. Don’t rely on your doctor to catch everything-they often have only 10-15 minutes per visit. Pharmacists specialize in this.

Erica Cruz
November 13, 2025 AT 11:01Ugh, another ‘educational’ post that reads like a textbook chapter someone copied and pasted into Reddit. I get it, DDIs are important-but do we really need 2,000 words to explain that grapefruit juice + statins = bad? I’ve been on simvastatin for 5 years and my pharmacist flagged this in 2 seconds. The real issue? Most people don’t even know what’s in their medicine cabinet. And no, ‘natural’ doesn’t mean safe. St. John’s Wort? More like St. John’s *Worst*.
Also, why does every article about meds feel like it’s written by a pharmacologist who hates fun?
Johnson Abraham
November 14, 2025 AT 15:51lol so grapefruit juice messes with ur meds? wow i had no idea. i drink it every mornin with my pills. guess im gonna die soon 😅
also why do docs always act like we’re dumb? i just want to know if i can take tylenol with my blood pressure stuff. why’s it so hard?!
Shante Ajadeen
November 14, 2025 AT 17:30This was actually super helpful. I’ve been on 7 different meds since my heart surgery last year and I always feel overwhelmed. The part about pharmacists catching 37% of DDIs? That’s a game-changer. I’m scheduling a med review next week-I never thought to ask. Thanks for breaking it down without making me feel stupid. You’re the reason I still trust healthcare.
Also, I just told my mom to stop taking St. John’s Wort with her antidepressants. She didn’t know. We all need more of this kind of info.
Ps: Grapefruit juice is officially banned in my house now. 😅
dace yates
November 15, 2025 AT 05:45Interesting. I’m curious-how much of the variability in DDI outcomes is actually due to gut microbiome differences versus genetic factors? The post mentions both, but the microbiome section feels underdeveloped. Are there any large-scale studies correlating specific bacterial strains with altered drug metabolism? I’ve read a few papers on digoxin inactivation, but nothing comprehensive. Would love to see a follow-up on this.
Also, how do these interactions play out in patients with IBD or post-bariatric surgery? Absorption changes could make even ‘safe’ combos risky.
Danae Miley
November 16, 2025 AT 13:49The claim that ‘80–90% of DDI alerts are false’ is misleading without context. False positives aren’t the problem-poorly designed alert systems are. The real failure is in clinical workflow integration. If your EHR throws 47 pop-ups during a 10-minute visit, of course clinicians ignore them. This isn’t user error; it’s system failure.
Additionally, the FDA’s ‘weak, moderate, strong’ classification is outdated. It ignores cumulative effects, polypharmacy, and renal/hepatic impairment. A ‘weak’ interaction in a 78-year-old with CKD stage 3 is not weak-it’s catastrophic. We need dynamic, patient-specific risk scoring, not static thresholds.
And yes-grapefruit juice is still dangerous. Don’t be that person.
Charles Lewis
November 16, 2025 AT 17:11It is both a privilege and a profound responsibility to engage with the topic of drug-drug interactions, as these phenomena represent not merely biochemical phenomena, but deeply human consequences-lives altered, families disrupted, healthcare systems strained by preventable errors.
The complexity of cytochrome P450 metabolism, the subtlety of transporter inhibition, the silent danger of herbal supplements-these are not abstract concepts reserved for academic journals. They are the quiet killers in suburban living rooms, in nursing homes, in emergency departments where a simple OTC cold remedy becomes the catalyst for a cardiac arrest.
It is imperative, therefore, that we approach this issue not merely with clinical precision, but with compassion, with education, and with systemic reform. The burden should not rest solely on the patient to memorize a list of forbidden foods and supplements. Rather, we must design healthcare environments where safety is engineered into the workflow-where pharmacists are not afterthoughts but integral members of the care team, where electronic systems are intelligent, not intrusive, and where every clinician, from the intern to the attending, understands that a single interaction can undo months of therapeutic progress.
And yes, grapefruit juice remains a villain. But so too does complacency.
Renee Ruth
November 17, 2025 AT 18:38Okay but let’s be real-this whole ‘drug interaction’ thing is just a scam to make pharmacists and big pharma rich. I’ve been taking 12 meds since 2018 and I’ve never had an issue. Everyone’s just scared of pills now. My cousin took St. John’s Wort with her antidepressants and she’s fine. She’s even happier now. Maybe your body just adapts?
Also, why are we blaming grapefruit juice? It’s the FDA’s fault for approving bad drugs in the first place. And why do they even make drugs that interact? Are they trying to kill us?
And don’t even get me started on ‘genetics.’ I’m not getting my DNA tested just to take ibuprofen. This is dystopian nonsense.
Also, I’ve been on warfarin for 8 years and I eat spinach every day. I’m fine. So… maybe stop scaremongering?
Samantha Wade
November 19, 2025 AT 13:26Thank you for this comprehensive, meticulously researched overview. It is rare to encounter such clarity on a subject that is so often muddled by misinformation. The emphasis on pharmacist-led interventions is particularly vital-pharmacists are the most underutilized resource in preventive medicine, and their role in mitigating DDIs is not merely supportive, it is foundational.
I would like to add that the rise of direct-to-consumer genetic testing has created a new layer of complexity. Patients are bringing raw genetic data to their providers without context, often misinterpreting variants like CYP2D6 poor metabolizer status as a definitive contraindication rather than a risk modifier. This underscores the urgent need for clinical decision support tools that integrate genomics, pharmacy records, and real-time lab values-not just static alerts.
Additionally, I encourage all readers to advocate for medication reconciliation at every transition of care. A 2023 JAMA study showed that patients who received structured medication reviews during hospital discharge had a 41% reduction in 30-day readmissions due to DDIs. This is not theoretical. It is actionable. And it saves lives.
Finally: grapefruit juice is not a snack. It is a pharmacological wildcard. Treat it as such.