When you hear low-dose CT, a type of computed tomography scan that uses significantly less radiation than a standard CT scan. Also known as low-dose CT scan, it's not meant to replace full scans—it's designed for routine screening in people at higher risk for certain diseases, especially lung cancer. Unlike traditional CT scans that capture detailed images for diagnosis, low-dose CT is about catching problems early, before symptoms show up. It’s the same machine, same technology, but with adjusted settings that cut radiation exposure by up to 80%.
This isn’t just a minor tweak—it’s a game-changer for people with a history of smoking, long-term exposure to pollutants, or a family history of lung cancer. Major health groups like the U.S. Preventive Services Task Force recommend annual low-dose CT scans for adults aged 50 to 80 who’ve smoked at least 20 pack-years and either still smoke or quit within the last 15 years. That’s over 8 million people in the U.S. alone who could benefit. The goal? Catch tumors when they’re small, treatable, and before they spread. Studies show that regular low-dose CT screening can reduce lung cancer deaths by up to 20% in high-risk groups.
It’s not just for lungs. Doctors are starting to use low-dose CT for other screening purposes too—like checking for coronary calcium buildup to assess heart disease risk, or monitoring people with a history of certain cancers for early signs of recurrence. The key advantage? Speed, safety, and sensitivity. A scan takes less than 10 seconds. No needles. No fasting. You just lie still while the machine spins around you. And because it’s so sensitive, it can spot nodules as small as a few millimeters—something a regular chest X-ray would miss entirely.
But it’s not perfect. False positives happen. A small spot on the scan might turn out to be harmless scar tissue or an old infection. That’s why follow-up tests, like repeat scans or biopsies, are often needed. That’s also why it’s not recommended for everyone. If you’ve never smoked, have no other risk factors, and are under 50, the risks of unnecessary testing likely outweigh the benefits. Radiation, even at low levels, adds up over time. The trick is knowing who it helps—and who it doesn’t.
What you’ll find in the articles below is a practical mix of real-world advice: how to prepare for a low-dose CT, what your results mean, how often you should get one, and what alternatives exist if you’re not a candidate. You’ll also see how it compares to other screening tools, what doctors look for in the images, and how insurance and policy changes are making this test more accessible. There’s no fluff—just clear, direct info from people who’ve been through it, or who’ve studied it closely. If you’re considering this scan—or already had one—these posts will help you understand what comes next.
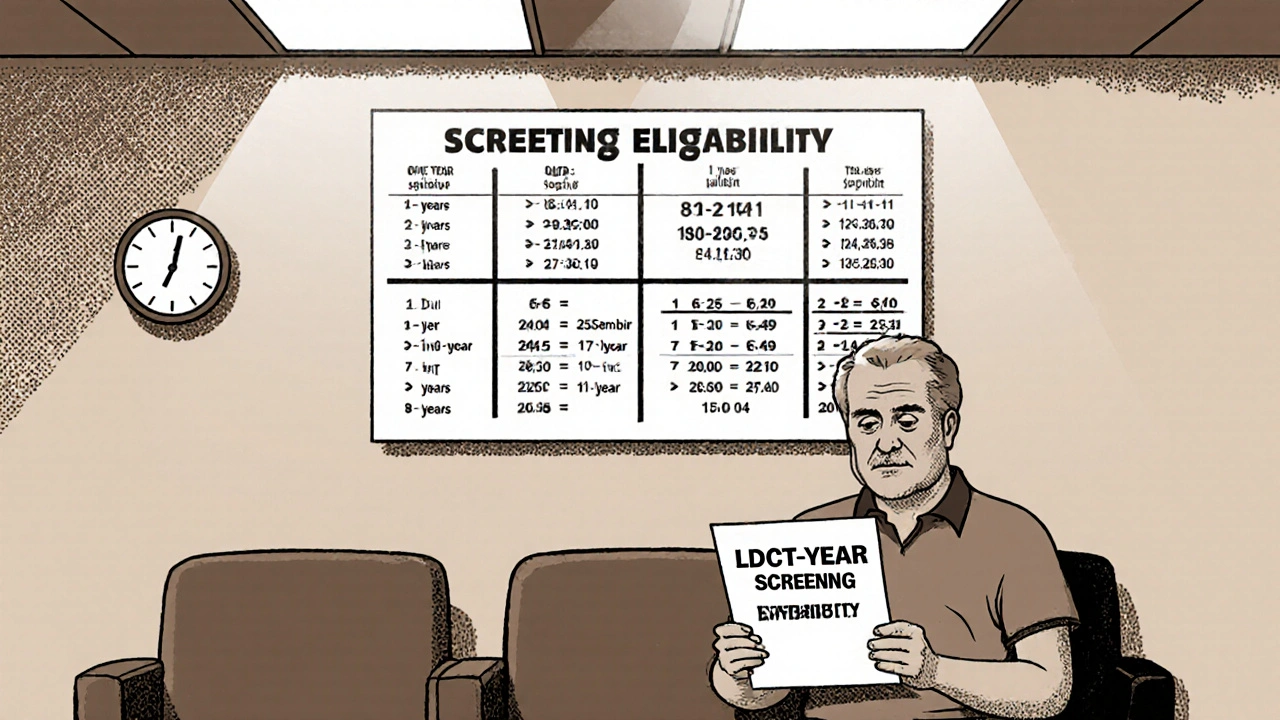
Low-dose CT screening can save lives in smokers by catching lung cancer early. Learn who qualifies, how it works, the real risks, and what to do next.

Compare Waklert (armodafinil) with modafinil, Adrafinil, Adderall, and natural alternatives to find the safest, most effective option for focus and alertness. Learn what works, what doesn’t, and why.

Struggling with lung inflammation can make even basic activities feel exhausting. Luckily, there are simple home remedies that can help calm inflammation and support lung health. Some everyday foods and easy habits can make a real difference. This article sorts out what actually works, from steam therapy to anti-inflammatory herbs. Give your lungs a break without having to run to the pharmacy.
Want generic Clomid cheap online? Here’s how to do it safely and legally in 2025-prices, telehealth, legit pharmacies, red flags, and smarter alternatives.
Explore the latest research, new formulations, and future directions for metoclopramide, including safety updates, combination therapies, and personalized dosing.

Discover how to soothe tendonitis pain naturally with ice, heat, stretches, strengthening exercises, and anti‑inflammatory herbs for lasting relief.