Why Smokers Need to Talk About Lung Cancer Screening
If you’re a current or former smoker, especially if you’ve smoked for years, you’ve probably heard about lung cancer. But hearing about it and actually doing something about it are two very different things. The truth is, lung cancer kills more people in the U.S. than colon, breast, and prostate cancers combined. And for people who smoked, the risk doesn’t just go away when they quit. That’s why low-dose CT (LDCT) screening isn’t just an option-it’s one of the most effective ways to catch lung cancer early, when it’s still treatable.
Who Qualifies for Low-Dose CT Screening?
The rules changed in 2021, and they’re simpler than you might think. If you’re between 50 and 80 years old, and you’ve smoked at least 20 pack-years, you qualify. A pack-year means smoking one pack a day for a year. So if you smoked two packs a day for 10 years, that’s 20 pack-years. Or one pack a day for 20 years. It adds up faster than you’d expect.
And here’s the key: you still qualify if you quit smoking, but only if it’s been less than 15 years since you stopped. Once you’ve been smoke-free for 15 years or more, the screening benefit drops off. Also, if you have a serious health condition that limits your life expectancy to less than 10 years, or if you wouldn’t be able to have surgery if cancer were found, screening isn’t recommended.
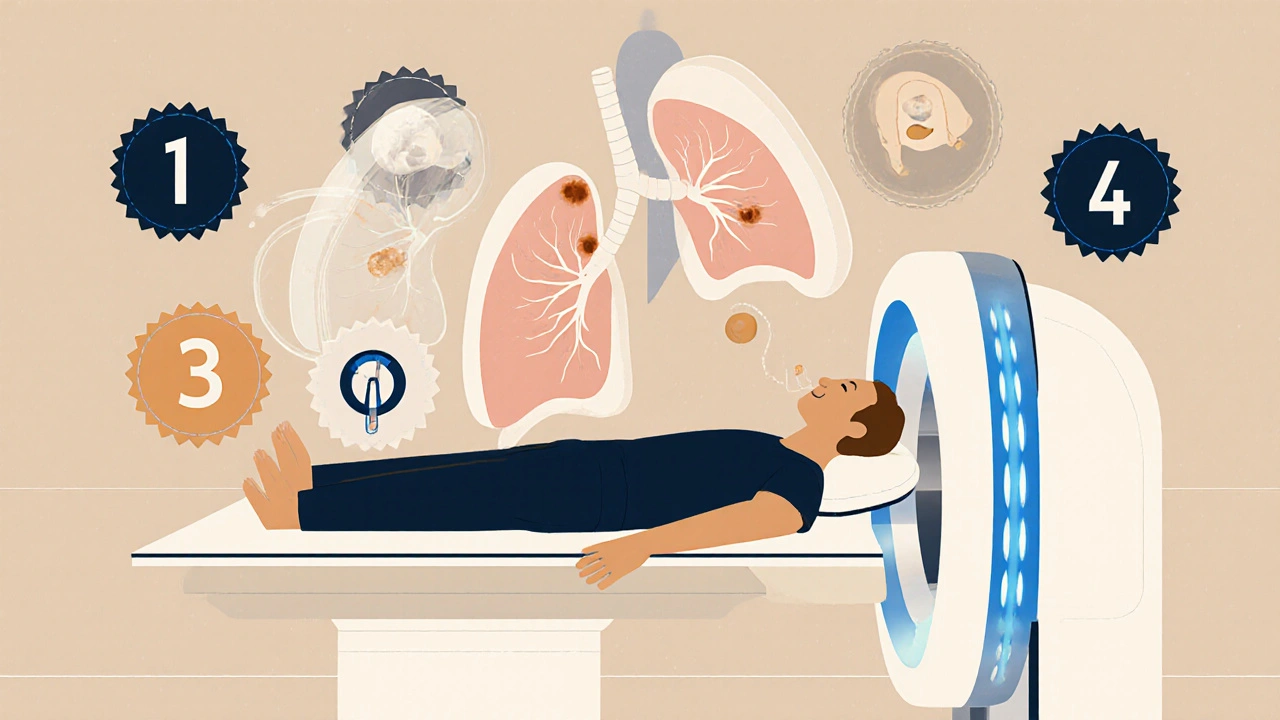
How Does Low-Dose CT Work?
Unlike a regular chest X-ray, which gives a flat image, LDCT takes detailed 3D pictures of your lungs in under 10 minutes. You lie on a table, breathe in, hold your breath for a few seconds, and that’s it. No needles, no fasting, no prep. The radiation dose is about 1.5 millisieverts-roughly the same as a mammogram or a third of what you get from a standard CT scan. It’s low, but not zero. That’s why screening is only recommended for people who truly need it.
The goal isn’t to find every little shadow. It’s to catch the ones that could become cancer. And it works. The National Lung Screening Trial showed that annual LDCT screening reduced lung cancer deaths by 20% compared to chest X-rays. That’s not a small win. It’s life-changing.
The Real Trade-Offs: False Positives and Anxiety
Here’s the part no one talks about enough: LDCT finds a lot of things that aren’t cancer. About 14% of people who get screened will have a finding that looks suspicious. But most of those turn out to be harmless-scar tissue, old infections, or just normal variations in lung structure.
Still, when you get called back for another scan, or a biopsy, it’s scary. One study found that 37% of people with false positives had moderate to severe anxiety that lasted more than six months. That’s real emotional toll. And while follow-up tests are usually safe, they add cost, time, and stress. That’s why the screening isn’t a one-size-fits-all test. It’s a decision you make with your doctor after talking through the risks and benefits.
What Your Doctor Should Talk About Before You Get Screened
Medicare and the U.S. Preventive Services Task Force both require a shared decision-making visit before you can get screened. That means your provider needs to spend 20 to 30 minutes with you-not just hand you a referral. They should explain:
- That screening reduces your chance of dying from lung cancer by about 1.5% to 2% over 10 years
- That about 1 in 7 people will get a false positive result
- That some cancers found might never have caused harm (overdiagnosis)
- That you need to keep getting screened every year until you no longer qualify
If your doctor skips this step, ask for it. This isn’t a routine test like a flu shot. It’s a serious health tool that needs context.
What Happens After the Scan?
Results are rated using Lung-RADS, a standard system that tells doctors what to do next. Here’s what the categories mean:
- Lung-RADS 1: Negative. No nodules. Come back next year.
- Lung-RADS 2: Benign findings. Like calcified spots. Come back next year.
- Lung-RADS 3: Probably benign. Small nodule, low risk. Come back in 6 months.
- Lung-RADS 4: Suspicious. Needs follow-up in 3 months or biopsy. Subdivided into 4A (low suspicion), 4B (moderate), and 4X (high suspicion).
Most people fall into categories 1 or 2. Only a small fraction get a 4, and even fewer need surgery. But knowing the system helps you understand what’s happening if you’re called back.
Why So Few Smokers Are Getting Screened
Here’s the hard truth: even though 14.5 million Americans now qualify for LDCT screening, only about 8% actually get it. That’s not because people don’t care. It’s because of access.
Many people don’t know they’re eligible. Others say their doctor never mentioned it. In one survey, 42% of eligible patients said their provider never brought it up. Some live far from accredited centers-there are only about 1,842 in the entire U.S., and they’re mostly in cities. One Reddit user drove 127 miles just to get screened. Others can’t take time off work or don’t have reliable transportation.
And there’s a racial gap: Black smokers have higher lung cancer rates but are 20% less likely to be screened than White smokers. That’s not a coincidence. It’s a system failure.
What’s New in 2025?
Technology is catching up. In 2023, the FDA approved the first AI tool for LDCT analysis-LungAssist by VIDA Diagnostics. Early results show it cuts false positives by over 15%. That means fewer unnecessary biopsies and less anxiety.
Doctors are also starting to use better risk models. The PLCOm2012 tool doesn’t just look at pack-years. It adds in family history, coughing, wheezing, and even education level. That helps identify who’s at the highest risk and who might benefit most from screening.
Still, the core message hasn’t changed: if you smoke or used to smoke, and you’re 50 or older, ask your doctor about LDCT. It’s not magic. But it’s one of the few tools we have that actually saves lives.
What to Do Next
If you think you qualify:
- Calculate your pack-years: (cigarettes per day / 20) × years smoked
- Check if you’re between 50 and 80
- Confirm you quit smoking less than 15 years ago (if applicable)
- Ask your doctor: "Am I eligible for low-dose CT screening?"
- If they say no, ask why. If they say yes, schedule the screening
Don’t wait for symptoms. Lung cancer rarely causes pain or coughing until it’s advanced. By then, it’s too late.
Screening Isn’t a Cure-It’s a Lifeline
One woman from Ohio, 53, got her LDCT scan after 25 pack-years of smoking. The scan found a stage 1 tumor. She had surgery. Five years later, she’s cancer-free. She says she’s alive because she got screened.
But she’s the exception, not the rule. Most people who qualify never get screened. That’s not because they don’t care. It’s because the system is broken. The good news? You can fix it for yourself. Ask the question. Make the call. Show up for the scan. Your lungs-and your future-depend on it.

Nikhil Purohit
November 20, 2025 AT 19:46Debanjan Banerjee
November 22, 2025 AT 14:10Steve Harris
November 23, 2025 AT 11:57Shawn Sakura
November 24, 2025 AT 15:28Daisy L
November 25, 2025 AT 17:15Anne Nylander
November 26, 2025 AT 12:36Franck Emma
November 26, 2025 AT 20:41Noah Fitzsimmons
November 27, 2025 AT 02:56Sammy Williams
November 27, 2025 AT 19:09Julia Strothers
November 28, 2025 AT 16:41Erika Sta. Maria
November 30, 2025 AT 16:33Cooper Long
December 2, 2025 AT 05:40Sheldon Bazinga
December 2, 2025 AT 14:39