When you see an drug expiration, the date printed on a medicine label indicating when the manufacturer guarantees full potency and safety. Also known as expiration date, it’s not just a marketing trick—it’s a scientifically tested limit based on how the active ingredients break down over time. Most people assume expired drugs turn toxic, but that’s not usually true. The real issue is they lose strength. A 2012 FDA study found that 90% of more than 100 drugs, both prescription and over-the-counter, were still effective even 15 years past their expiration date—when stored properly. But that doesn’t mean you should keep every pill you’ve ever bought.
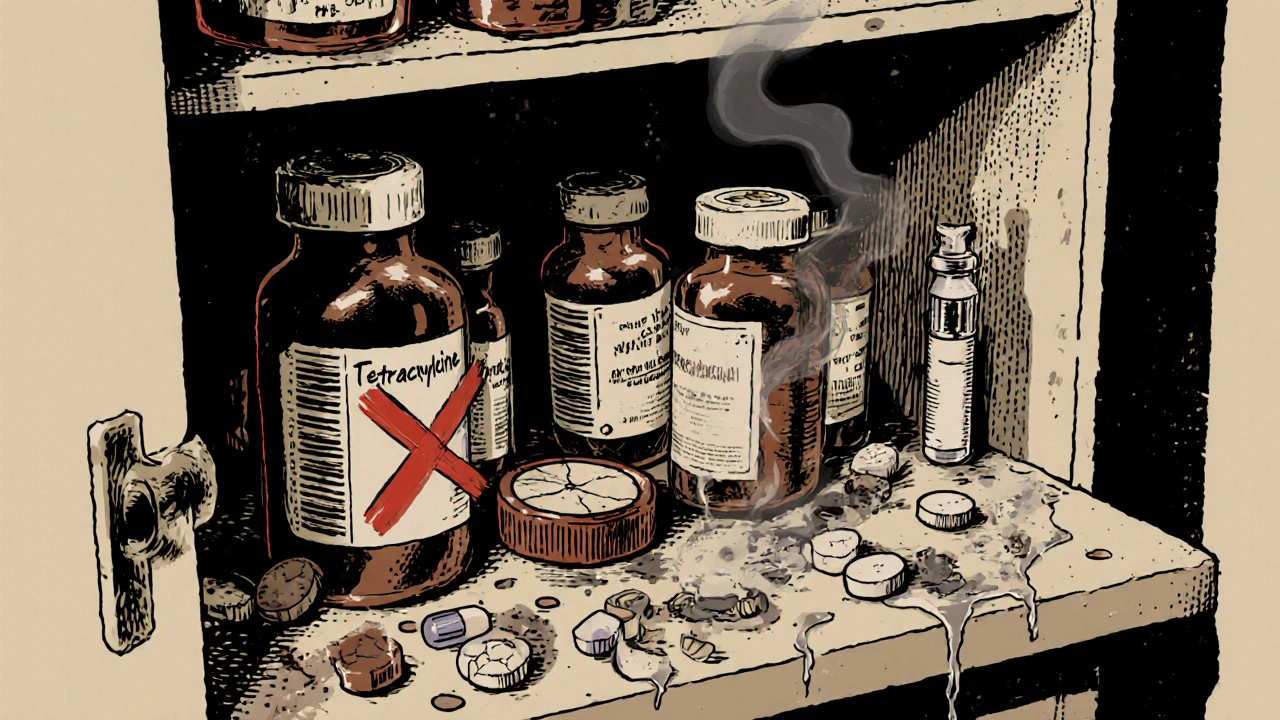
What actually makes a drug expire isn’t just time—it’s medication storage, how and where you keep your drugs at home. Heat, humidity, and light degrade pills faster than the clock. Storing antibiotics in a bathroom cabinet? That’s a bad idea. Moisture turns tablets into mush and makes capsules stick together. Insulin, epinephrine auto-injectors, and liquid antibiotics? Those can become dangerous fast if they get too warm. expired medication, drugs past their labeled expiration date aren’t always harmful, but they’re unreliable. If your asthma inhaler doesn’t spray right, or your allergy pill doesn’t stop the sneezing, you’re not getting the dose you need.
There’s also the risk of contamination. Once a bottle is opened, bacteria or mold can grow, especially in liquids or creams. Antibiotics like amoxicillin suspension can turn into a breeding ground after just 14 days—even if the bottle says the expiration is two years away. And don’t forget about kids and pets. A child mistaking an old painkiller for candy is a real emergency, no matter how old the pill is.
So what should you do? First, check your medicine cabinet. Look for pills that are discolored, cracked, or smell funny. Liquid meds that look cloudy or separated? Toss them. Second, store meds right—cool, dry, dark places like a bedroom drawer, not the kitchen or bathroom. Third, don’t hoard. Buy only what you need. If you’re not using a drug regularly, it’s probably not worth keeping past its date.
The FDA and most pharmacists agree: when in doubt, throw it out. Especially for life-saving meds like nitroglycerin, EpiPens, or insulin. A weak dose could cost you your health—or your life. And if you’re worried about waste, many pharmacies and local health departments offer safe disposal programs. No need to flush pills or toss them in the trash where kids or wildlife might find them.
Below, you’ll find real-world guides on how to handle expired drugs safely, how to store medicines properly, and which ones you should never risk using—even if they look fine. These aren’t theoretical tips. They’re based on what doctors, pharmacists, and real patients have learned the hard way.
Check your medicine cabinet twice a year to remove expired drugs and prevent accidents. Learn what to toss, where to store meds safely, and how to dispose of them the right way.

Learn practical diet and nutrition strategies to keep estradiol levels balanced, covering phytoestrogens, omega‑3s, vitamin D, fiber and more.

Medicare can now negotiate drug prices for the first time under the Inflation Reduction Act. Discover how this cuts costs for seniors, changes insurer discounts, and reshapes the entire U.S. drug pricing system.

A clear comparison of Cleocin Gel (clindamycin) with other topical acne treatments, covering how they work, price, side effects, and tips for choosing the best option.
Authorized generics are the exact same drug as the brand-name version, made by the same company, but sold under a generic label. Learn how they work, why they exist, and how to spot them to save money without sacrificing quality.
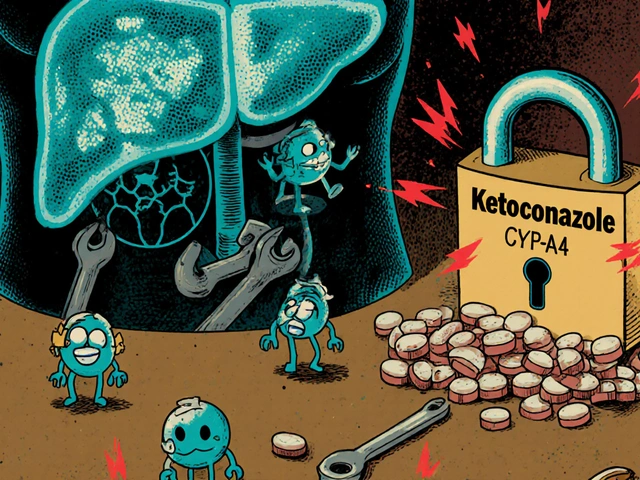
Drug-drug interactions can cause serious harm when medications clash in your body. Learn how liver enzymes, transporters, and genetics affect drug safety, and what you can do to avoid dangerous combinations.