Ever wonder why a doctor sometimes gives a pill that attacks many germs at once? That’s a broad-spectrum antibiotic. It’s designed to kill a wide range of bacteria, so it can handle infections when the exact bug isn’t known yet. While it’s a handy tool, using it the wrong way can spark resistance, making future infections harder to treat.
These meds target basic bacterial processes that most germs share—like cell‑wall building or protein production. Because the target is common, the drug can knock out several species in one go. Common examples include amoxicillin, ciprofloxacin, and doxycycline. Doctors often start with one of these when a patient shows signs of a respiratory infection, urinary tract infection, or skin infection but the lab hasn’t identified the culprit yet.
Think of it like a universal key that fits many locks. It’s convenient, but the key can also open doors you didn’t intend to lock, affecting good bacteria in your gut. That’s why you might notice stomach upset or yeast overgrowth after a course.
Broad-spectrum antibiotics shine in emergency rooms, where time is short and the infection source is unclear. They’re also useful for mixed infections—cases where more than one type of bacteria is involved, such as certain abdominal infections.
However, if a lab test shows a specific bug, a narrow‑spectrum antibiotic (like penicillin for streptococcal throat) is usually better. It targets the germ directly and leaves more of your friendly microbes alone. Swapping to a narrow option can also cut down the chance of resistance developing.
Here are quick rules to follow:
Remember, antibiotics only work on bacterial infections. They won’t help with colds, flu, or most sore throats caused by viruses.
Using broad-spectrum antibiotics wisely protects you and the community. When you understand why a doctor chose a particular drug, you can follow the treatment plan with confidence and avoid unnecessary side effects.
Got more questions about a specific antibiotic or how it fits into your health plan? PharmaCorner’s database lets you look up detailed info on drugs like amoxicillin, clindamycin, and many others. Stay informed, ask your healthcare provider, and keep those germs in check.

A detailed look at Chloramphenicol, its clinical uses, safety concerns, and how it stacks up against common alternatives such as Azithromycin, Ciprofloxacin, and Doxycycline.
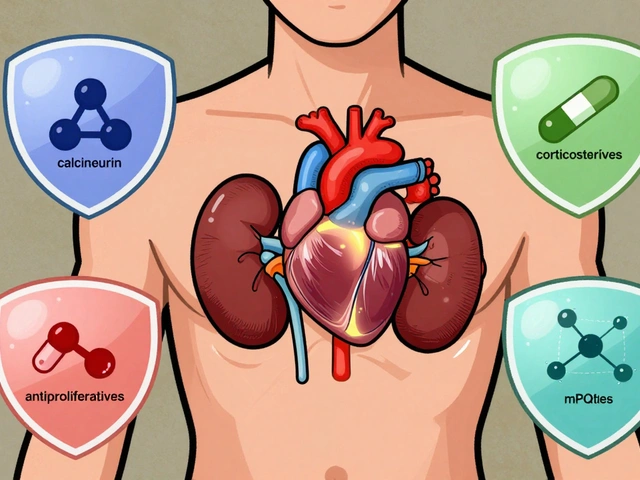
Immunosuppressants prevent organ rejection after transplant but carry serious risks like infection, cancer, and kidney damage. Learn how to manage these drugs safely, avoid missed doses, and reduce long-term side effects.

The nocebo effect explains why people feel side effects from medications even when the drug has no active ingredient. Expectations, not chemistry, often drive these reactions - and they're more common than you think.
Topical steroids treat eczema and psoriasis effectively but can cause skin thinning if misused. Learn how to use them safely with the right dose, duration, and strength to avoid permanent damage.

Learn how clinician portals and apps help healthcare providers detect adverse drug reactions in real time. Discover which tools work best for hospitals, clinical trials, and low-resource settings-and how to use them without burnout.

Learn how cabergoline works for men, the conditions it treats, dosing tips, benefits, risks, and how it compares to other dopamine agonists.