Topical steroids are one of the most common treatments for eczema, psoriasis, and other inflammatory skin conditions. Used correctly, they work fast - often clearing redness and itching in just a few days. But when misused, they can cause skin thinning, bruising, stretch marks, and even permanent damage. The problem isn’t the medication itself. It’s how it’s used.
What Are Topical Steroids, Really?
Topical corticosteroids are anti-inflammatory drugs applied directly to the skin. They’re not the same as the oral or injected steroids athletes misuse. These creams, ointments, and gels target inflammation right where it happens - without flooding your whole body with hormones. Skin cells break down most of the steroid before it can enter your bloodstream, which is why they’re safer than pills.
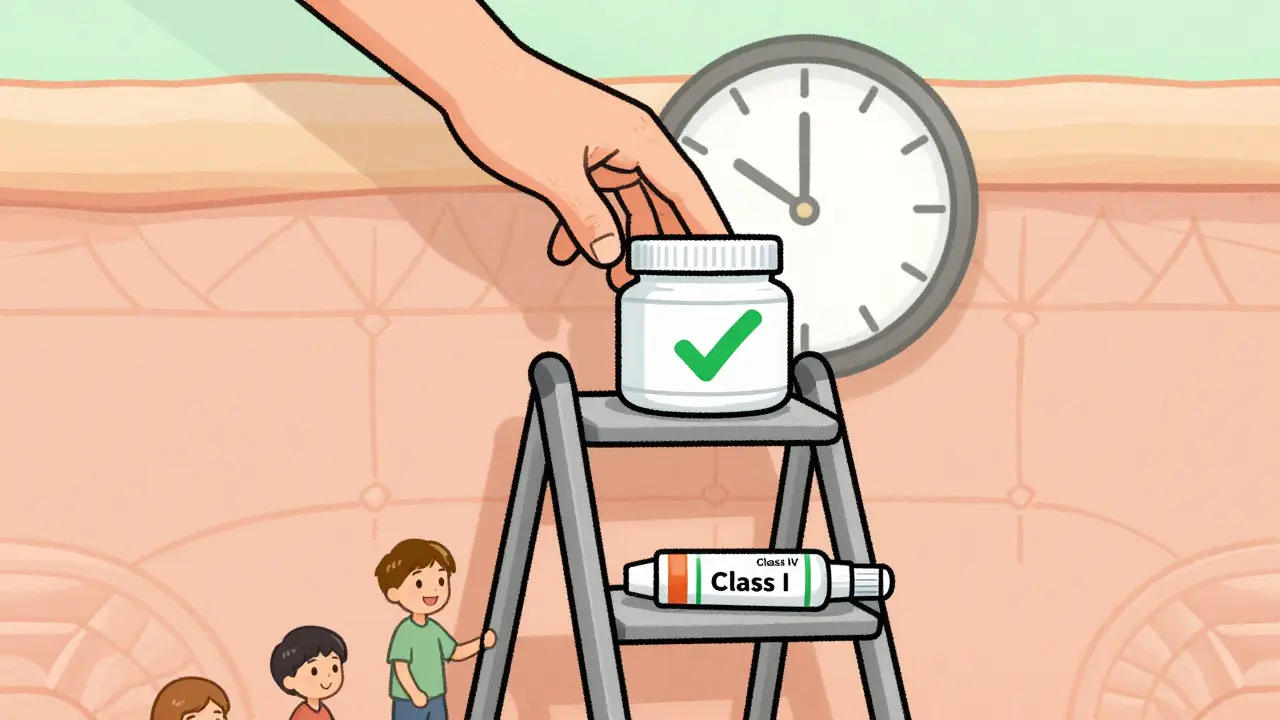
They’ve been around since the 1950s and are still the first-line treatment for millions of people. In the U.S., about 40% of all dermatology prescriptions are for topical steroids. Hydrocortisone, the mildest version, is even sold over the counter. But strength matters. There are seven potency levels, from super-potent (Class I) to low-potency (Class VII). A cream that works wonders on thick, scaly skin on your elbows could wreck your eyelids if used there.
Why Skin Thinning Happens - And Where It’s Most Likely
Skin thinning, or atrophy, is the most feared side effect. It doesn’t happen overnight. It builds up over weeks or months of daily use, especially with stronger formulas. The steroid breaks down collagen and elastin - the proteins that keep skin firm and resilient. Once it’s gone, the skin becomes fragile, transparent, and prone to tearing or bruising.
Some areas are far more vulnerable than others. The face, neck, armpits, groin, and inner thighs have naturally thin skin. That’s why guidelines say: never use anything stronger than mild potency on your face, especially near the eyes. Prolonged use there can lead to cataracts, glaucoma, or a red, bumpy rash around the mouth called perioral dermatitis.
Even worse, people often apply strong steroids to the folds of skin - behind the knees, under the arms - because that’s where eczema flares worst. That’s a dangerous combo: high potency + thin skin + long duration = high risk of atrophy. One Reddit user described how months of self-treating eczema with a potent steroid led to visible stretch marks and skin that tore when he scratched. He didn’t realize he was damaging his skin until it was too late.
The Right Way to Use Them - Dose, Frequency, and Duration
Most people use too much or too often. Studies show patients either under-apply (thinking less is safer) or over-apply (thinking more works faster). Both backfire. Under-dosing prolongs the flare. Over-dosing raises side effect risks.
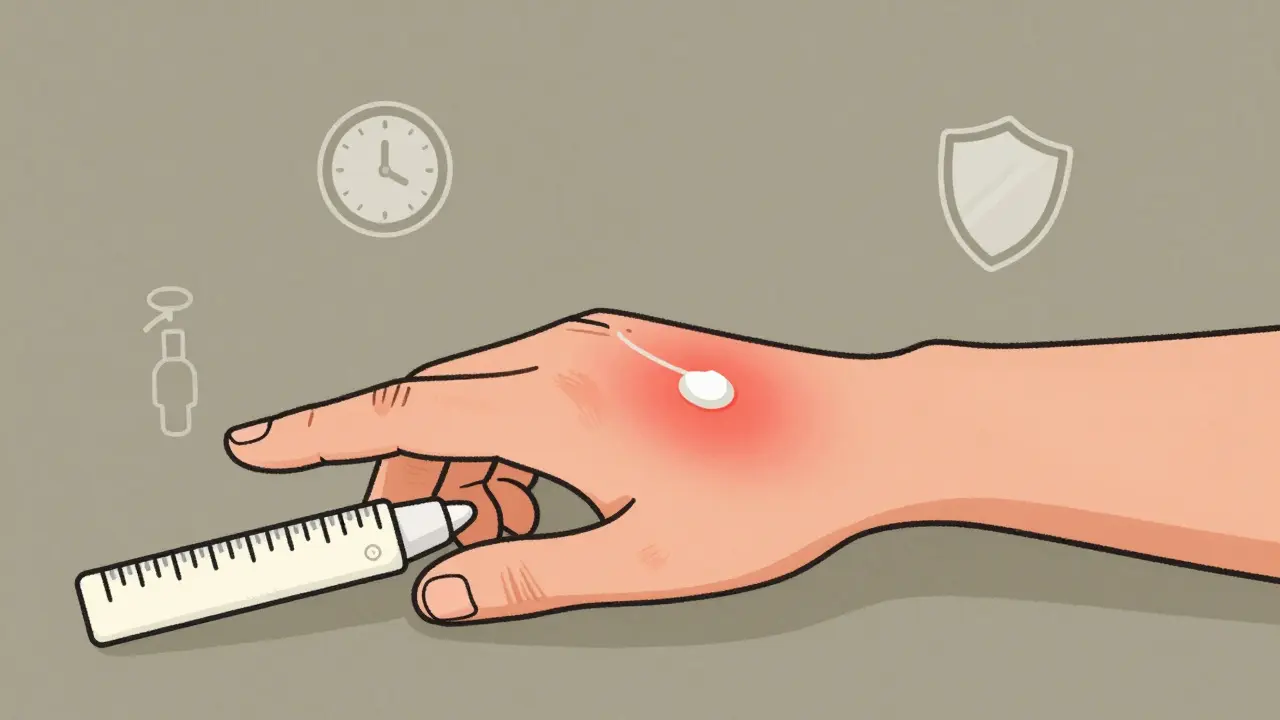
The solution? Fingertip units (FTUs). One FTU is the amount of cream or ointment that fits on the tip of your index finger, from the first crease to the tip. It’s not a glob. It’s a thin line.
- One FTU covers an area about the size of two adult hands (front and back)
- One arm needs 3 FTUs
- One leg needs 6 FTUs
- One foot needs 2 FTUs
- Face and neck? No more than 0.5 to 1 FTU total
Apply only once a day - even for strong steroids. Applying twice doesn’t help. It just increases the chance of skin thinning. The American Academy of Family Physicians says there’s no evidence that more than once daily helps, and plenty of proof that it harms.
Duration matters even more than dose. Super-potent steroids should never be used for more than two weeks. Even moderate ones shouldn’t go beyond four weeks without a doctor’s check-in. If your skin isn’t better in 10-14 days, something else is wrong. Don’t keep applying more.

Step-Down Therapy: The Smart Way to Avoid Long-Term Damage
Many people think once they start a steroid, they have to keep using it. That’s not true. The smart approach is called step-down therapy.
Start with the strongest steroid that fits your condition and body area - but only for a short burst. For example: use a Class II steroid on your arms for 10 days to knock down the flare. Then switch to a Class IV or V for another week. Then switch to a mild steroid or non-steroidal cream like tacrolimus. Finally, stop altogether and rely on moisturizers.
Dr. Jonathan Silverberg, a leading eczema specialist, says this method works better than long-term low-dose use. It controls symptoms fast and reduces the chance of side effects. The National Eczema Society reports that patients who follow this approach rarely develop skin thinning.
What to Avoid - And What to Do Instead
Here’s what not to do:
- Don’t use strong steroids on your face, eyelids, or genitals unless a doctor specifically says so
- Don’t cover the area with plastic wrap or tight clothing to ‘boost’ the effect
- Don’t use leftover steroid cream from last year’s flare - potency fades, and you might be using the wrong strength
- Don’t use steroids for itching alone. If there’s no redness or swelling, you don’t need them
Here’s what to do instead:
- Always use a moisturizer - but wait 20-30 minutes after applying steroid before putting it on
- Wash your hands before and after applying to avoid spreading the cream to other areas
- Keep a log: note what you used, how much, and for how long
- See your doctor if you’ve used a steroid for more than two weeks without improvement
Alternatives When Steroids Are Too Risky
Not everyone can use steroids. People with sensitive skin, children, or those needing long-term control often need other options.
Calcineurin inhibitors like tacrolimus and pimecrolimus are non-steroidal creams that work well on the face and folds. They don’t cause skin thinning. But they’re pricier and can cause a burning sensation at first. Crisaborole is another option for mild eczema - it’s an ointment that reduces inflammation without steroids.
These alternatives are growing in use. In 2023, the UK’s NHS and the FDA both updated guidelines to encourage them for sensitive areas. But cost remains a barrier. Many patients still default to steroids because they’re cheaper and covered by insurance.
When to Worry - Signs of Steroid Damage
Not every red spot means damage. But here are warning signs you need to see a doctor:
- Skin looks transparent or wrinkled, like parchment paper
- Easy bruising - even from light pressure
- Visible stretch marks (striae) where none existed before
- Red, bumpy rash around the mouth or nose
- Blurred vision or eye pain after using steroids near the eyes
- Rebound flare - worse than before - when you stop using the cream
Rebound flares are a red flag. They often mean you’ve been using steroids too long or too strong. Stopping suddenly can trigger a severe reaction. Always taper off under medical guidance.
The Bottom Line: Steroids Are Tools, Not Crutches
Topical steroids aren’t evil. They’re powerful tools - like a scalpel. Use them right, and they save skin. Use them wrong, and they ruin it.
The American Academy of Dermatology says clearly: "When used appropriately under medical supervision, the benefits of topical corticosteroids significantly outweigh the risks." But that’s only true if you follow the rules.
Use the lowest strength that works. Apply only once a day. Use the right amount - one FTU at a time. Limit use to two to four weeks. Step down to milder options. Talk to your doctor before restarting.
There’s no shame in needing them. But there’s real risk in guessing. Skin thinning is permanent. Don’t let a quick fix become a long-term problem.
Can topical steroids cause permanent skin thinning?
Yes, if used incorrectly - especially high-potency steroids on thin skin areas like the face, groin, or armpits for more than 2-4 weeks. Once collagen breaks down, the skin doesn’t fully recover. Early signs like transparency or easy bruising mean you need to stop and see a doctor.
How much steroid cream should I use?
Use fingertip units (FTUs). One FTU - the amount from the first crease to the tip of your index finger - covers an area about the size of two adult hands. For the face and neck, use no more than half to one FTU total. More doesn’t help. It only raises side effect risks.
Is it safe to use steroid cream on my face?
Only mild potency (Class VI or VII) for short periods - no more than 5-7 days. Never use medium or strong steroids on your face. The skin there is thin and absorbs more. Risks include acne, red rashes around the mouth, and eye damage like glaucoma or cataracts.
Can I use steroid cream every day for months?
No. Even low-potency steroids shouldn’t be used daily for more than 4 weeks without medical supervision. Long-term daily use increases the risk of skin thinning, stretch marks, and rebound flares. Always follow a step-down plan: start strong, then reduce strength and frequency.
What should I do if my skin gets worse after stopping steroid cream?
This is called steroid withdrawal or rebound. It often happens after prolonged, unsupervised use. Don’t restart the cream. See a dermatologist. You may need a different treatment plan, including non-steroidal creams or gradual tapering under supervision. Rebound flares can be severe but are manageable with proper care.

Stephen Craig
January 4, 2026 AT 06:39Used hydrocortisone on my eyelids for a week because my eczema flared. Didn’t think twice. Woke up one morning and my skin looked like tissue paper. Took months to recover. Never again. Stick to the FTU rule. Less is everything.
It’s not about fear. It’s about respect for the tool.
Connor Hale
January 5, 2026 AT 21:38The real tragedy isn’t the misuse-it’s that people are left to self-diagnose and self-treat because access to dermatologists is a luxury. I’ve seen moms using Class II steroids on their toddlers’ faces because the clinic waitlist is six months. This isn’t negligence. It’s systemic failure.
Roshan Aryal
January 6, 2026 AT 04:07Oh wow, another American medical pamphlet dressed up like wisdom. You people treat steroids like they’re sacred scripture. Meanwhile, in India, we’ve been using turmeric paste, neem oil, and cold compresses for centuries-no skin atrophy, no rebound flares, no FTU math. Your ‘science’ is just corporate pharmacy with a white coat.
And don’t get me started on ‘step-down therapy.’ Sounds like a corporate flowchart designed to keep you buying more cream.
Jack Wernet
January 6, 2026 AT 23:59While I appreciate the thoroughness of this post and its adherence to evidence-based guidelines, I must emphasize the ethical imperative of patient education. The disparity between clinical recommendations and real-world practice is not merely a matter of compliance-it reflects a broader failure in health literacy dissemination. The fingertip unit concept, though elegant in theory, remains inaccessible to populations without visual aids or medical guidance. We must do better.
Jennifer Glass
January 7, 2026 AT 10:03I used a steroid cream for my hands for 3 weeks straight because I was tired of the itching. When I stopped, my skin felt like it was screaming. I didn’t know it was rebound until I Googled it at 2 a.m. Now I keep a little logbook-what I used, when, how much. It’s weirdly calming. Like a diary for my skin.
Jacob Milano
January 7, 2026 AT 10:29Just want to say this is the most helpful thing I’ve read all year. I used to think steroids were the cure-all-until my inner thighs turned into translucent parchment. Now I use tacrolimus, moisturize like my life depends on it (it does), and actually sleep at night. No magic, just consistency. And yes, FTUs are real. I measure mine with a ruler now. No shame.
Vikram Sujay
January 7, 2026 AT 16:07It is of profound importance to recognize that the adoption of topical corticosteroids must be contextualized within the cultural and socioeconomic realities of the patient. The concept of the fingertip unit, while scientifically sound, presupposes a level of health literacy and access to measurement tools that are not universally available. In rural communities, where visual demonstrations are scarce and medical terminology is alien, a simple, culturally resonant analogy-such as the size of a pea or the width of a thumbnail-may prove more effective than clinical jargon. Education must meet people where they are.
Jay Tejada
January 9, 2026 AT 07:44So let me get this straight-we’re supposed to use a tiny line of cream, wait 30 minutes to moisturize, and not use it longer than two weeks… but the doctor gives me a 60-day supply and says ‘use as needed’? Yeah, right. This whole system is designed to keep us hooked. I’m just glad I figured it out before I looked like a ghost.