Nocebo Risk Calculator
This tool estimates your potential risk of experiencing nocebo effects (side effects caused by negative expectations) based on factors discussed in the article.
Research shows women report 23% more side effects, people with anxiety are 1.7x more likely to experience nocebo symptoms, and negative communication increases risk by up to 40%.
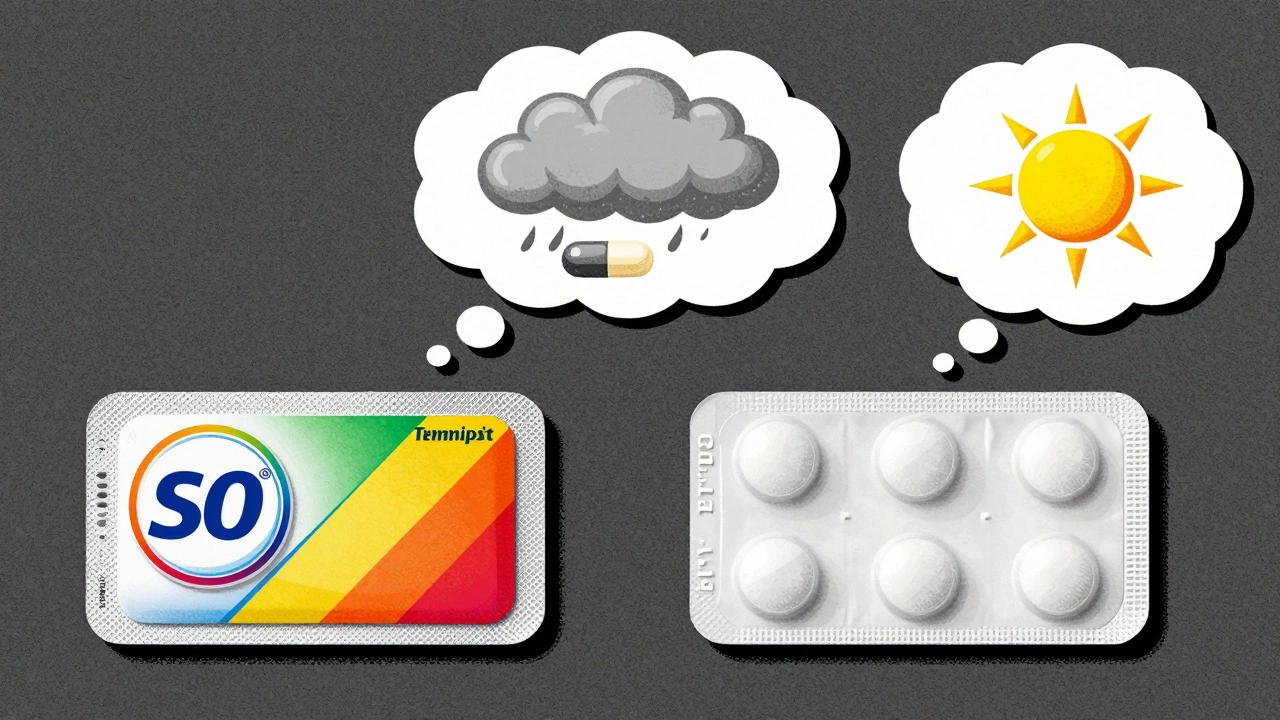
Imagine taking a pill that doesn’t contain any active ingredient - just sugar or water - and still feeling sick. Headache. Nausea. Fatigue. You didn’t get poisoned. The drug didn’t react with your body. But your brain? It convinced your body something was wrong. That’s the nocebo effect.
What Exactly Is the Nocebo Effect?
The nocebo effect isn’t imagination. It’s real. Your brain, under the influence of negative expectations, triggers physical symptoms - even when there’s no chemical cause. The word comes from Latin: nocebo means “I will harm.” It’s the dark twin of the placebo effect, where positive beliefs make treatment work better. But here, the belief is that something bad is coming. In clinical trials, about 20% of people taking a sugar pill report side effects. Around 10% drop out of studies because they feel worse. And these aren’t people with mental health issues. These are everyday patients. Their bodies are responding to what they’ve been told, not to any drug. It’s not just about pills. It happens with injections, patches, even generic medications. A patient switches from brand-name sertraline to a generic version - same active ingredient, same dosage - and suddenly feels dizzy and anxious. They go back to the brand name, and the symptoms vanish. The drug didn’t change. Their expectation did.How Your Brain Creates Real Symptoms
Your brain doesn’t distinguish between real threats and imagined ones. When you’re told, “This medicine can cause severe nausea,” your mind starts scanning your body for signs of nausea. You feel a slight stomach flutter - normal after eating - and suddenly it’s proof the drug is working against you. Neuroscience shows this isn’t just psychology. Brain scans reveal that negative expectations light up areas tied to pain and discomfort: the anterior cingulate cortex, the insula, the prefrontal regions. These are the same areas that activate when you actually experience pain. Your body isn’t faking it. It’s responding to a signal your brain sent out. Studies on remifentanil, a powerful painkiller, showed this clearly. When patients were told the drug would make them more sensitive to pain after its effects wore off, their pain didn’t just return - it got worse. The drug’s pain-relieving power vanished. All because of what they were told.Why Some People Are More Susceptible
Not everyone gets hit by the nocebo effect the same way. Certain people are more vulnerable:- Women report 23% more side effects than men in placebo groups - not because their bodies react differently, but because they’re more likely to notice and report subtle changes.
- People with anxiety or depression are 1.7 times more likely to experience nocebo symptoms.
- Those who are pessimistic or highly attuned to health information - especially if they’ve had bad experiences with meds before - are prime targets.
- Patients who read long, scary medication leaflets? They’re more likely to report side effects that match what’s listed.
Doctors, Leaflets, and the Language That Hurts
Healthcare providers often mean well. But how they talk about side effects can backfire. Saying, “Some people get nausea, dizziness, and fatigue” sounds neutral. But it plants the idea. Patients start watching for those symptoms. They find them. They blame the drug. Research shows that changing how you phrase things reduces nocebo effects. Instead of: “This medicine can cause headaches in up to 15% of users,” try: “Most people tolerate this medicine well. A small number may feel a mild headache, but it usually passes quickly.” Patient information leaflets are a major problem. They list every possible side effect - even ones that occur in 1 in 10,000 people. They don’t say which are common, which are rare, or which are likely unrelated. A 2019 study found that the more side effects listed, the more patients reported them - even if they were taking a placebo. In the UK, NHS pilot programs trained doctors to use balanced communication. They cut medication discontinuation rates by 14%. It wasn’t about hiding risks. It was about framing them in a way that didn’t scare people into feeling worse.Generics, Brand Switches, and the Power of Packaging
The generic drug market is worth over $200 billion. But it’s plagued by nocebo effects. Patients believe brand-name drugs are “stronger” or “better.” So when they switch, they expect trouble - and they get it. Reddit threads are full of stories like this: “I switched to generic fluoxetine and got brain zaps. I switched back to the brand and they vanished.” The active ingredient? Identical. The pills? Same shape, same size, same manufacturer in many cases. But the color, the logo, the name - they triggered the brain’s expectation loop. Pharmaceutical companies know this. That’s why some generics look almost identical to brand-name versions - not just for marketing, but to reduce the nocebo effect. The body doesn’t care about the label. But the mind does.
What Can You Do About It?
If you’re starting a new medication:- Ask your doctor: “What’s the chance this will cause real side effects versus just feeling like it does?”
- Don’t read the leaflet before you start. Read it after - when you’ve had time to adjust.
- Keep a simple journal: Note how you feel, but don’t assume every twinge is from the drug.
- If symptoms appear, wait a week. Many “side effects” fade as your body adapts.
- If you’re switching brands, tell your pharmacist you’re concerned about nocebo. They’ve seen it before.
- Don’t list every possible side effect. Focus on common ones and reassure patients that most won’t happen.
- Use positive framing: “Most people feel fine” instead of “Some people feel bad.”
- Normalize minor symptoms: “It’s normal to feel a little tired at first. That usually goes away.”
- Be aware of your tone. A worried expression or hesitant voice can trigger more than your words.
The Bigger Picture: Why This Matters
The nocebo effect isn’t just about feeling bad. It’s about real-world consequences:- 15-20% of patients stop taking effective medications because they think they’re causing side effects - when the real cause is their expectation.
- People switch drugs unnecessarily, increasing costs and risking worse outcomes.
- Healthcare systems waste billions on avoidable consultations, tests, and replacements.
Final Thought: Your Mind Is Part of the Medicine
You can’t control everything about your health. But you can control how you interpret it. The nocebo effect reminds us that medicine isn’t just chemistry. It’s conversation. It’s trust. It’s belief. A pill doesn’t cure you alone. Your mind helps - or hurts - the process. The goal isn’t to ignore risks. It’s to understand them without letting fear rewrite your body’s story.Can the nocebo effect cause real physical damage?
The nocebo effect doesn’t cause permanent organ damage or disease. But it can trigger real physiological responses - increased heart rate, muscle tension, stress hormones, and pain sensitivity - that mimic illness. These symptoms are temporary and fade when expectations change. However, if they lead to stopping effective treatment, that can cause long-term harm.
Are nocebo effects the same as psychosomatic symptoms?
They’re closely related, but not identical. Psychosomatic symptoms arise from psychological stress without a clear trigger. Nocebo effects are specifically tied to expectations about a medical treatment. The trigger is information - a warning, a label, a doctor’s tone. The mechanism is the same: brain → body response. But the context is different.
If I feel side effects from a generic drug, does that mean it’s weaker?
No. Generic drugs must meet the same bioequivalence standards as brand-name versions. If you feel worse after switching, it’s likely due to expectation, not chemistry. Many patients report side effects that disappear when they’re told the generic is identical. This is a classic nocebo pattern.
Can you get nocebo effects from over-the-counter meds?
Absolutely. People often report headaches, drowsiness, or stomach upset from common painkillers like ibuprofen or acetaminophen - even when they’ve taken them before without issue. If they read a warning label or heard a friend say “this gives me nausea,” their brain may trigger the same response. The effect works on any treatment, branded or not.
Is it unethical to downplay side effects to avoid nocebo?
No, as long as you’re still giving honest, balanced information. Ethical communication isn’t about hiding risks - it’s about avoiding fear-based framing. Saying “most people feel fine” instead of “many get nausea” doesn’t mislead. It prevents unnecessary panic. Informed consent doesn’t require scaring people. It requires clarity and context.
Do placebos and nocebos work the same way in the brain?
Yes - and that’s why they’re two sides of the same coin. Both activate the brain’s expectation pathways. Placebos trigger reward systems and pain-relief chemicals like endorphins. Nocebos activate stress and pain pathways like cortisol and substance P. The same brain regions light up - just in opposite directions. Your mind is running the show, whether you’re feeling better or worse.



val kendra
December 3, 2025 AT 19:30Elizabeth Crutchfield
December 5, 2025 AT 12:06Ben Choy
December 6, 2025 AT 03:34Emmanuel Peter
December 8, 2025 AT 02:08Ashley Elliott
December 9, 2025 AT 17:32Chad Handy
December 10, 2025 AT 12:18Augusta Barlow
December 12, 2025 AT 07:03Joe Lam
December 13, 2025 AT 00:07Scott van Haastrecht
December 13, 2025 AT 02:35Chase Brittingham
December 14, 2025 AT 10:55Bill Wolfe
December 14, 2025 AT 20:16Ollie Newland
December 15, 2025 AT 23:53Rebecca Braatz
December 17, 2025 AT 03:17Michael Feldstein
December 17, 2025 AT 22:22jagdish kumar
December 18, 2025 AT 01:42Benjamin Sedler
December 18, 2025 AT 14:12zac grant
December 18, 2025 AT 15:32michael booth
December 20, 2025 AT 05:52Carolyn Ford
December 20, 2025 AT 21:56