When someone gets a transplanted organ, their body sees it as an invader. That’s where anti-rejection drugs, medications that suppress the immune system to prevent it from attacking a transplanted organ. Also known as immunosuppressants, they’re not optional—they’re life-sustaining. Without them, even a perfectly matched kidney, heart, or liver can be destroyed by the body’s own defenses in days.
These drugs don’t just block one thing. They hit multiple parts of the immune system. cyclosporine, a cornerstone transplant drug that stops T-cells from triggering rejection, has been used for decades. But newer options like tacrolimus, a more potent alternative with fewer long-term side effects than cyclosporine are now first-line for many patients. Both require regular blood tests to make sure levels stay in the narrow window where they work—without causing kidney damage or infections.
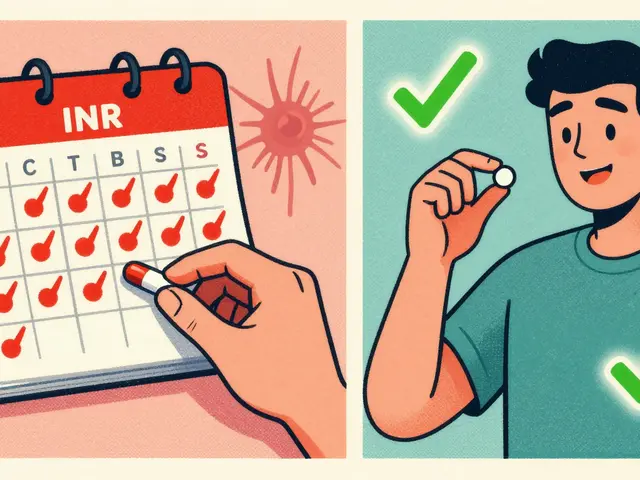
Anti-rejection drugs don’t come with a one-size-fits-all plan. Your dose depends on your organ, your age, your other meds, and even your genetics. Some people need three or four drugs at once. Others, years after transplant, can drop down to just one. But skipping a dose—even once—is risky. A missed pill can trigger rejection, and that’s not something you can afford to wait on. It’s not like missing a vitamin. It’s like turning off your body’s safety system.
These drugs also play into bigger issues you might not think about. Like how generic versions can behave differently in your body, especially with narrow therapeutic drugs. Or how alcohol, grapefruit, or even herbal supplements can throw off your levels. And if you’re on these meds long-term, you’re more vulnerable to infections, skin cancers, and high blood pressure. That’s why tracking your meds, knowing your triggers, and talking to your transplant team isn’t just good advice—it’s survival.
You’ll find posts here that dig into the real-world side of these drugs: how they interact with other medications, why some people react differently to generics, how storage and timing matter, and what alternatives exist when side effects become too much. These aren’t theoretical discussions. They’re based on what patients and doctors deal with every day.
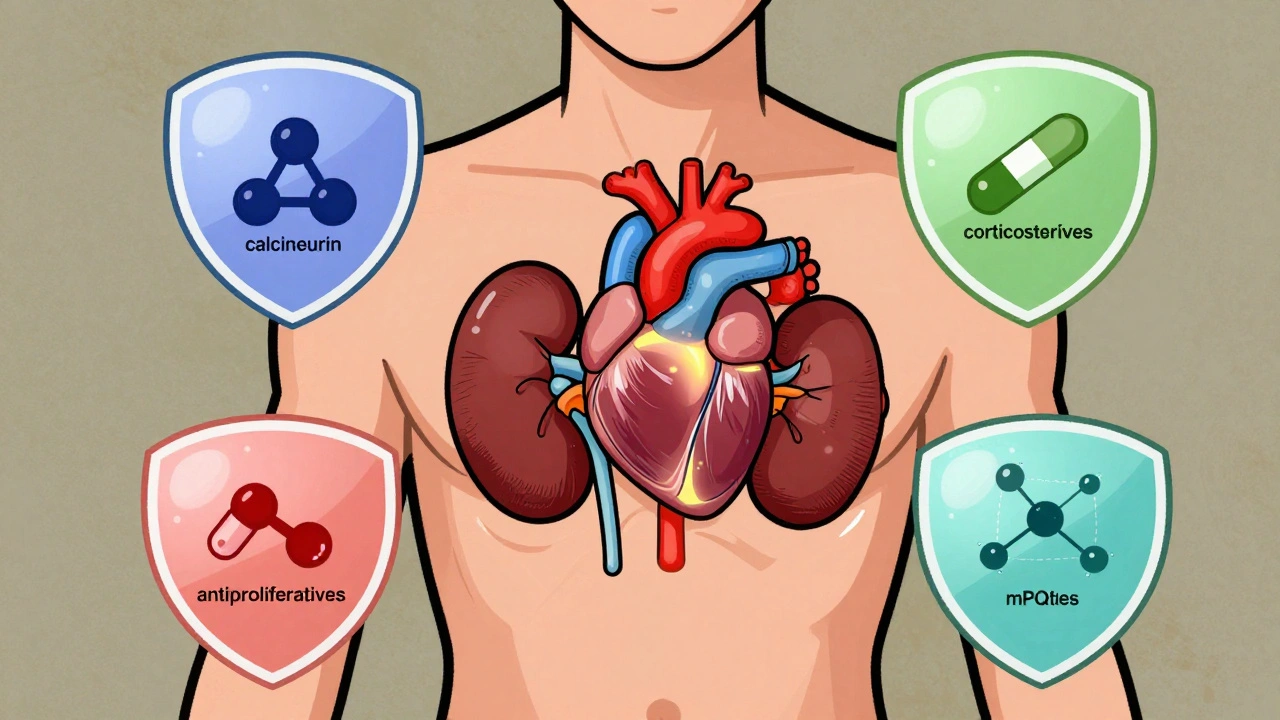
Immunosuppressants prevent organ rejection after transplant but carry serious risks like infection, cancer, and kidney damage. Learn how to manage these drugs safely, avoid missed doses, and reduce long-term side effects.

Learn the daily foot inspection checklist proven to prevent diabetic foot ulcers and avoid amputation. Follow evidence-based steps for washing, inspecting, moisturizing, and choosing safe footwear every day.
Warfarin and DOACs are both blood thinners used to prevent clots, but DOACs are now preferred for most patients due to better safety, fewer interactions, and no need for regular blood tests. Learn the key differences and what to do in an emergency.

Compare Waklert (armodafinil) with modafinil, Adrafinil, Adderall, and natural alternatives to find the safest, most effective option for focus and alertness. Learn what works, what doesn’t, and why.

Bronchiectasis causes chronic cough and mucus buildup, leading to frequent infections. Daily airway clearance and targeted antibiotics can break this cycle, slow lung damage, and improve quality of life - even if the condition can't be cured.
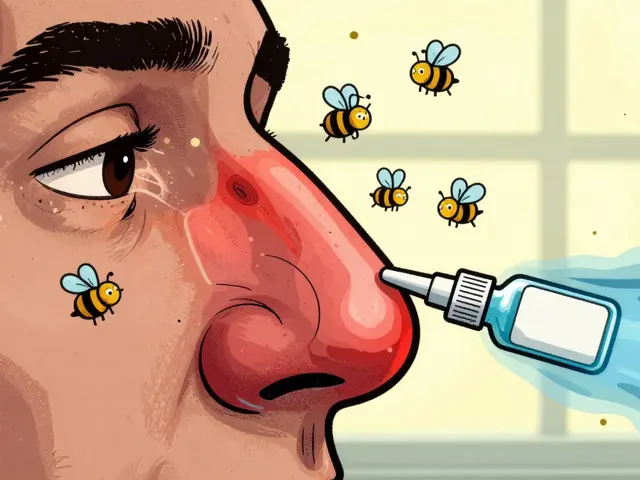
Nasal steroid sprays are the most effective treatment for allergic rhinitis, reducing inflammation to relieve congestion, sneezing, and runny nose. Learn how they work, why daily use matters, and how to use them safely.