Biosimilar Substitution Checker
This tool helps you determine if interchangeable biosimilars can be substituted in your state. Remember: the FDA approves interchangeability, but state laws control substitution. As of 2023, 47 states allow substitution under specific conditions.
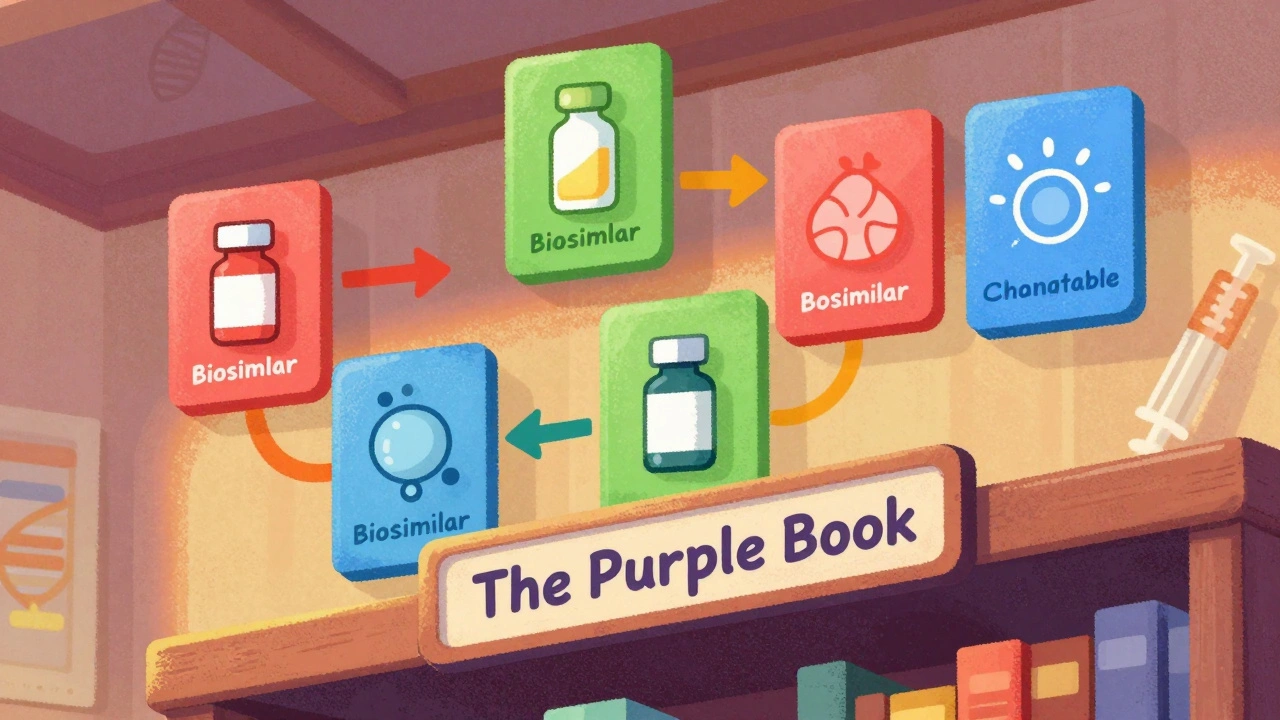
The Purple Book isn’t a novel you read for fun-it’s the FDA’s official, searchable database that tells you exactly which biological drugs are approved, which ones are biosimilars, and which ones can be swapped out like generics. If you’re a pharmacist, a prescriber, or even a patient trying to understand why your insulin changed, this is the resource that holds the answers. Unlike the Orange Book for small-molecule drugs, the Purple Book deals with complex biological products-drugs made from living cells, like insulin, rheumatoid arthritis treatments, and cancer therapies. And because these drugs aren’t simple chemical copies, the rules around substitution are more complicated. That’s where biosimilars and interchangeability come in.
What the Purple Book Actually Contains
The Purple Book lists every FDA-licensed biological product, including the original reference products and their biosimilar or interchangeable versions. It’s not just a list-it’s a structured database with color-coded product cards. Each card shows the brand name, the generic name, the date it was approved, and whether it’s a reference product (351(a)), a biosimilar (351(k)), or an interchangeable biosimilar (also 351(k), but with extra designation). The color matching is key: if two products have the same color card, one is biosimilar or interchangeable with the other. This makes it easy to spot which drugs are linked.
It also includes details like whether the product had exclusivity protection when it launched, what delivery systems it uses (like autoinjectors or pre-filled syringes), and whether it’s regulated by CDER (drugs) or CBER (biologics like vaccines and cell therapies). Since 2020, the FDA merged two separate lists into one searchable platform, fixing years of confusion. Before that, you had to check two different databases. Now, you type in a drug name-say, Humira-and instantly see all the biosimilars approved to match it, along with which ones can be swapped without a doctor’s permission.
Biosimilar vs. Interchangeable: The Key Difference
All interchangeable products are biosimilars, but not all biosimilars are interchangeable. That’s the most important thing to remember.
A biosimilar is a biological product that’s highly similar to its reference drug. The FDA requires extensive testing to prove there are no clinically meaningful differences in safety, purity, or potency. That means it works the same way in the body. But being similar isn’t enough to allow automatic substitution at the pharmacy.
An interchangeable biosimilar goes further. To earn that label, the manufacturer must prove that switching back and forth between the biosimilar and the original drug doesn’t increase risk or reduce effectiveness. This isn’t just one study-it’s multiple switching studies where patients alternate between the two drugs over time. The FDA wants to see that the outcome stays the same whether you start with the brand, switch to the biosimilar, switch back, or keep switching. If the results are consistent, the FDA grants the interchangeable designation.
Here’s the catch: the FDA doesn’t say interchangeable biosimilars are better or safer. They just say they’re predictable when swapped. A non-interchangeable biosimilar works just as well in practice, but you can’t automatically substitute it unless your state law and prescriber allow it.
Why Interchangeability Matters for Pharmacists
Pharmacists are on the front lines of drug substitution. If a doctor prescribes Humira, and there’s an interchangeable biosimilar available, the pharmacist can legally swap it without calling the doctor-if state law permits it. But here’s where it gets messy: federal law says the FDA can approve interchangeability, but state law controls whether substitution actually happens.
As of 2023, 47 states and Puerto Rico allow pharmacists to substitute interchangeable biosimilars without prescriber approval. But even in those states, rules vary. Some require the pharmacist to notify the prescriber. Others require patient consent or documentation. A few states still require the prescriber to specifically write “dispense as written” on the prescription to block substitution.
This patchwork creates real-world confusion. A patient in California might get an interchangeable biosimilar automatically. The same patient in New York might get the brand-name drug unless the doctor explicitly allows substitution. The Purple Book tells you what’s federally approved-but it doesn’t tell you what your state allows. That’s why pharmacists need to know both the federal designation and their state’s pharmacy laws.

What’s in the Purple Book Right Now?
As of late 2023, only seven biosimilars had earned the interchangeable designation from the FDA. That’s out of dozens of approved biosimilars. The interchangeable ones include:
- Two insulin products (used for diabetes)
- Three treatments for inflammatory diseases like rheumatoid arthritis and Crohn’s disease
- Two eye treatments for retinal conditions
These are high-cost drugs where substitution could save billions. But the approval process is slow. Manufacturers have to run extra studies, and the FDA reviews them carefully. The number of interchangeable products is expected to grow, but it’s not happening overnight.
It’s also worth noting: the Purple Book doesn’t list “unbranded biologics.” Some companies market biosimilars without brand names, calling them “equivalent.” But the FDA doesn’t consider those interchangeable unless they’ve gone through the full 351(k)(4) approval process. Just calling something “equivalent” doesn’t make it interchangeable under federal law.
How to Use the Purple Book Like a Pro
Using the Purple Book isn’t hard, but you need to know what you’re looking for. Here’s how:
- Go to the FDA’s Purple Book page (fda.gov/purplebook).
- Use the search bar to type in the brand name or generic name of a biological drug.
- Look at the results. Each product card shows its designation: 351(a), 351(k) Biosimilar, or 351(k) Interchangeable.
- Match the color of the product cards. If two cards are the same color, one is biosimilar or interchangeable with the other.
- Check the “Interchangeable” column-yes or no. If it says yes, that product can be substituted where state law allows.
- Click on the product to see its full approval history, including the date it was licensed and whether it had exclusivity.
Don’t rely on memory or outdated sources. The Purple Book is updated weekly. A product that wasn’t interchangeable last month might be today. Always check before dispensing.
What the FDA Isn’t Telling You
The FDA is clear: interchangeability doesn’t mean the drug is better. It just means switching won’t hurt. But in the real world, some prescribers still prefer the brand. Some patients worry about switching, even if it’s safe. And insurers often push for the cheapest option, which may not always be the interchangeable one.
Also, the Purple Book doesn’t include pricing. You can’t tell from the database which biosimilar is cheaper. That’s up to pharmacy benefit managers and insurers. The FDA’s job is to confirm safety and equivalence-not to set prices or control access.
Finally, the Purple Book doesn’t explain state laws. You need to check your state pharmacy board’s website separately. Some states have detailed guidance on substitution protocols, others don’t. That’s the hidden layer of complexity.
What’s Next for Biosimilars?
More biosimilars are coming. More will seek interchangeability. The FDA has issued draft guidance on labeling to make sure prescribers and pharmacists understand what each product can and can’t do. Companies are investing heavily in switching studies because the payoff is huge: if your biosimilar is interchangeable, it can be substituted automatically, just like a generic pill.
But the real barrier isn’t science-it’s perception. Many doctors and patients still think biosimilars are “less than.” The Purple Book helps by giving transparent, science-based data. But changing minds takes time. Education, clear labeling, and real-world outcomes will matter more than any database.
The Purple Book isn’t perfect. It doesn’t solve every problem. But it’s the most reliable source we have to understand what’s approved, what’s interchangeable, and what’s allowed. For anyone working with biological drugs, it’s not optional-it’s essential.
What is the Purple Book and who maintains it?
The Purple Book is an official, online database maintained by the U.S. Food and Drug Administration (FDA). It lists all FDA-approved biological products, including reference products, biosimilars, and interchangeable biosimilars. It was created under the Biologics Price Competition and Innovation Act (BPCIA) of 2010 and became a single searchable database in 2020.
What’s the difference between a biosimilar and an interchangeable product?
A biosimilar is highly similar to its reference drug with no clinically meaningful differences in safety or effectiveness. An interchangeable biosimilar meets all those requirements but also proves that switching back and forth between it and the original drug doesn’t increase risk or reduce effectiveness. Only interchangeable biosimilars can be automatically substituted at the pharmacy, subject to state law.
Can pharmacists substitute interchangeable biosimilars without a doctor’s permission?
It depends on state law. Federally, the FDA approves interchangeability, but states control whether substitution can happen. As of 2023, 47 states and Puerto Rico allow pharmacists to substitute interchangeable biosimilars without prescriber approval. However, some states require notification to the prescriber, patient consent, or documentation.
How many interchangeable biosimilars are approved as of 2023?
As of late 2023, the FDA had approved seven interchangeable biosimilars. These include two insulin products, three treatments for inflammatory diseases like rheumatoid arthritis, and two eye treatments for retinal conditions. More are expected as manufacturers complete additional clinical studies.
Does the Purple Book include pricing information?
No, the Purple Book does not include pricing or cost data. It only shows FDA approval status, product designations, and equivalence relationships. Pricing is determined by insurers, pharmacy benefit managers, and market competition, not the FDA.
Are unbranded biologics the same as interchangeable biosimilars?
No. The FDA does not consider unbranded biologics to be interchangeable biosimilars. An unbranded biologic may be equivalent in composition, but unless it has gone through the full 351(k)(4) approval process and received an interchangeable designation from the FDA, it cannot be substituted automatically at the pharmacy.
How often is the Purple Book updated?
The Purple Book is updated weekly. New approvals, designations, and updates to product information are added regularly. Always check the official FDA website for the most current data before making substitution decisions.


Kylee Gregory
December 5, 2025 AT 12:03The Purple Book is one of those quiet heroes of modern medicine-no hype, no ads, just cold, hard facts that keep us all honest. I’ve used it to double-check biosimilar substitutions for my elderly patients, and it’s saved us from a few scary mix-ups. It’s not glamorous, but it’s the glue holding together a system that could easily fall apart without transparency.
It’s funny how something so technical becomes so personal when you’re the one holding the prescription.
Still, I wish the FDA added a simple ‘Recommended for substitution’ flag next to the color codes. Not everyone has time to cross-reference state laws while juggling 20 prescriptions at 3 PM.
Chris Brown
December 5, 2025 AT 19:50Let’s be clear: the FDA’s obsession with ‘interchangeability’ is a bureaucratic mirage. The science is the same whether it’s labeled ‘interchangeable’ or not. This whole distinction exists because lawyers and insurers needed a checkbox to justify cost-cutting-not because patients need it.
Doctors still prescribe by name because they know, in practice, the difference is negligible. The Purple Book doesn’t fix the real problem: pharmaceutical monopolies disguised as innovation.
Also, ‘color-coded cards’? That’s not science. That’s a PowerPoint slide from 2007.
Michael Dioso
December 6, 2025 AT 12:06Oh please. You people act like the Purple Book is the Ten Commandments. It’s a database. A very nice one, sure-but it doesn’t make a biosimilar better. The real issue? Most prescribers don’t even know how to use it.
I’ve seen pharmacists swap interchangeable biosimilars and get yelled at by patients who think they’re getting ‘fake drugs.’ Meanwhile, the same patients pay $2,000 for a brand-name drug without blinking.
And don’t get me started on the 47 states with ‘substitution laws.’ That’s not healthcare policy-that’s a patchwork quilt stitched by drunk legislators.
Also, ‘unbranded biologics’? That’s just Big Pharma trying to sneak in generics under a new name. The FDA should shut that down. Full stop.
Krishan Patel
December 6, 2025 AT 20:08How can anyone claim this is a ‘transparent’ system when state laws override federal approval? This is not science-it is political theater dressed in lab coats.
The FDA approves interchangeability, but then a state in the Midwest decides that patients must sign a waiver just to receive a cheaper insulin? That’s not patient autonomy-that’s bureaucratic terrorism.
And you think color-coding helps? In India, we have 200+ biosimilars approved without any color system, and we don’t have chaos. Why? Because we trust our pharmacists and doctors-not a government database with a pretty UI.
Stop romanticizing bureaucracy. The real innovation is in the lab, not in the spreadsheet.
Carole Nkosi
December 7, 2025 AT 03:15I’ve watched my mother switch from Humira to a biosimilar after the Purple Book showed it was interchangeable. She was terrified. Said she’d rather pay double than risk ‘something happening.’
Turns out? She’s been on it for 18 months. No flare-ups. No side effects. No drama.
So why do we still treat biosimilars like second-class medicine? Because fear sells more than facts.
The Purple Book is just a mirror. It shows us what we’re too scared to believe: that science can be simple, affordable, and still safe.
Stop making it complicated. Just let people get better.
Annie Grajewski
December 7, 2025 AT 13:33so like… the purple book is just… a really fancy google doc??
i mean, i get it, it’s official and stuff, but like… why does it look like a 2012 wordpress site??
also, i clicked on ‘interchangeable’ for my insulin and it said ‘yes’ but my pharmacy still asked for a signature?? like… who’s lying here?? the fda or my pharmacist??
also, why is there no search by price?? i just wanna know which one’s cheaper, not which color it is 😭
Rupa DasGupta
December 9, 2025 AT 09:26OMG I JUST FOUND OUT MY RHEUMATOID ARTHRITIS DRUG IS INTERCHANGEABLE AND I DIDN’T EVEN KNOW 😭😭😭
my co-pay dropped from $180 to $35 and I cried in the pharmacy parking lot. Like, I’m not even joking. I had to call my sister to tell her.
But then I looked at the Purple Book and saw the color codes and was like… wait, is this the same one??
Then I called my pharmacist and she said ‘yes, honey, it’s the same stuff, just cheaper.’
So why does it take a database to make people feel like they’re getting a miracle??
Also, can we please make the website not look like it was built by a grad student in 2009? 🙏
William Chin
December 10, 2025 AT 11:13As a regulatory compliance officer with over 22 years in pharmaceutical oversight, I must emphasize that the Purple Book is not merely a reference tool-it is a foundational pillar of the BPCIA’s legislative intent. The distinction between biosimilar and interchangeable is not semantic; it is pharmacologically, legally, and ethically substantive. Failure to recognize this distinction constitutes a breach of professional responsibility.
Furthermore, the assertion that state laws are ‘patchwork’ is not only inaccurate but dangerously reductive. Each state’s pharmacy board operates under its own statutory authority, grounded in public health precedent. To dismiss this as ‘bureaucratic theater’ is to misunderstand the federalist structure of American medicine.
I urge all practitioners to consult the official FDA guidance documents, not Reddit comment threads, before making substitution decisions.
Harry Nguyen
December 11, 2025 AT 07:36Let’s be real-this whole ‘interchangeable’ thing is just the FDA letting Big Pharma off the hook. They approve a biosimilar, slap on ‘interchangeable,’ and now insurance companies can force patients to switch. Meanwhile, the original drug’s manufacturer just rebrands and hikes the price on the next version.
And don’t get me started on the color-coding. It’s like they’re trying to make a drug database look like a kindergarten poster.
Meanwhile, China and India are manufacturing better, cheaper biosimilars without all this red tape-and we’re stuck debating whether a green card means you can swap insulin.
Our system isn’t broken. It’s designed to protect profits, not patients.
Katie Allan
December 12, 2025 AT 08:35I want to thank the author for writing this. As a new pharmacist, I was overwhelmed by the complexity of biosimilars. The Purple Book felt like a maze until I read this.
One thing I’ve learned: patients don’t care about color codes or 351(k) designations. They care if their pain is managed and if they can afford it.
So I use the Purple Book to understand what’s allowed, then I talk to my patients. I say: ‘This is the same medicine, just less expensive. Would you like to try it?’
Most say yes. And that’s what matters.
Let’s not let bureaucracy steal our humanity.
Thank you for making this clear.
James Moore
December 13, 2025 AT 20:07Let me just say-this entire system is a masterclass in over-engineering. We have a biological drug that is, by all measurable clinical parameters, functionally identical to its reference product-yet we require a separate, additional, multi-year, multi-million-dollar clinical trial program just to label it ‘interchangeable’? And then, once we’ve spent all that money and time, we hand the decision of whether to actually substitute it over to 50 different state legislatures, each with their own arcane, inconsistent, and often contradictory rules?
Meanwhile, in the real world, a pharmacist in rural Nebraska, who has never even heard of the Purple Book, is handed a prescription for Humira, sees a cheaper biosimilar on the shelf, and just… swaps it anyway-because the patient can’t afford the brand, and the doctor isn’t around to say ‘no.’
So we’ve created a system that’s technically perfect, but practically irrelevant-and then we pat ourselves on the back for being ‘science-based.’
What we need is not more databases, more color codes, or more federal-state jurisdictional battles.
We need a single, national rule: if the FDA says it’s interchangeable, then it’s interchangeable. Period.
Everything else is just noise.
And yes-I’ve checked the Purple Book. Twice. And I still think this is ridiculous.
Kylee Gregory
December 13, 2025 AT 21:07William Chin just said it better than I ever could. The Purple Book isn’t broken-it’s being used wrong.
We treat it like a lawbook when it’s really a flashlight. It doesn’t tell you what to do-it tells you what’s possible.
The real work? Talking to patients. Explaining that ‘biosimilar’ doesn’t mean ‘second-rate.’
And yes, the website needs a redesign. But that’s the least of our problems.
Thanks for the clarity, William. I’m printing this out for my next team meeting.