When we talk about tricyclic antidepressants, a class of older psychiatric medications that work by balancing brain chemicals like serotonin and norepinephrine. Also known as TCAs, they were among the first drugs developed to treat depression and remain in use today—especially when newer options fail. Unlike SSRIs, which mostly target serotonin, tricyclics hit multiple neurotransmitters at once. That’s why they can help with more than just sadness—they’re also used for chronic pain, anxiety, insomnia, and even bedwetting in kids.
But they’re not simple to use. Side effects like dry mouth, weight gain, dizziness, and heart rhythm changes are common. Many patients stop taking them because the discomfort outweighs the benefit. That’s why doctors now often turn to SSRIs, a newer group of antidepressants with fewer side effects and safer profiles. Also known as selective serotonin reuptake inhibitors, they became the go-to in the 1990s and still are for most first-time users. Still, TCAs haven’t disappeared. For treatment-resistant depression, or when someone has nerve pain along with low mood, they can be the most effective tool left. Some studies show they work better than SSRIs for severe cases—but only if you can tolerate the side effects.
Another key player in this space is SNRIs, medications that increase both serotonin and norepinephrine, similar to TCAs but with cleaner action. Also known as serotonin-norepinephrine reuptake inhibitors, drugs like venlafaxine and duloxetine offer a middle ground: better effectiveness than SSRIs, fewer side effects than TCAs. If you’ve tried an SSRI and nothing changed, your doctor might skip straight to an SNRI instead of jumping to a TCA. But if cost is a concern—TCAs are often cheaper than brand-name SNRIs—they still hold value.
What you won’t find in most online lists is how personal this choice is. One person’s miracle drug is another’s nightmare. Some people with depression and migraines respond dramatically to amitriptyline, while others get so dizzy they can’t stand up. That’s why the posts below don’t just list drugs—they compare real-world outcomes, side effect burdens, and cost differences you won’t hear from a pharmaceutical rep.
Here, you’ll see how tricyclic antidepressants stack up against modern options—not in theory, but in practice. From how they affect sleep and energy to how they interact with heart meds and what alternatives actually work when TCAs don’t, this collection gives you the unfiltered details. No fluff. No marketing. Just what matters when you’re trying to feel better and stay safe.
Elavil (amitriptyline) is still used for pain, sleep, and depression, but many patients seek alternatives due to side effects. Compare duloxetine, pregabalin, mirtazapine, SSRIs, and non-drug options to find what works best for you.

Digestive enzyme supplements can help with specific GI conditions like EPI or lactose intolerance, but aren't a cure-all. Learn when they work, which ones to choose, and when to see a doctor instead.

Medicaid substitution rules prevent public insurance from replacing affordable private coverage. States vary widely in how they enforce these rules - some use waiting periods, others use real-time data. Learn how your state handles it and what changes came in 2024.

Most people don't tell their doctors about dietary supplements-even though they can interact dangerously with medications. Learn why full disclosure matters, which supplements are riskiest, and how to talk to your care team safely.
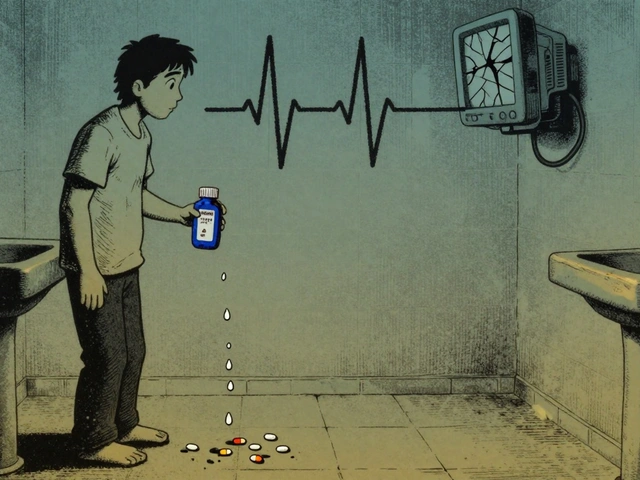
Loperamide, found in OTC antidiarrheals like Imodium, is being misused by people trying to self-treat opioid withdrawal. At high doses, it causes life-threatening heart rhythms and can be fatal. Learn the warning signs and why this isn't just another drug trend.

Explore how you can buy Neurontin online affordably. Understand the uses of gabapentin, potential side effects, typical dosages, and vital tip on drug interactions. This guide helps you make informed choices on medication while highlighting practical healthcare considerations.