Elavil Alternative Finder
What are your main concerns?
Select your primary issue to find the best alternatives
Key Considerations
- Drowsiness: Avoid if driving/operating machinery
- Weight gain: Average 2-5kg over 6 months
- Heart risk: Higher with existing heart conditions
- Withdrawal: Never stop abruptly
Elavil (amitriptyline) has been around since the 1960s, and for decades, it was one of the most prescribed antidepressants in the UK and US. But today, many patients and doctors are asking: is it still the best choice? With newer options available, and side effects like weight gain, dry mouth, and drowsiness that can be hard to live with, people want to know what else might work better - especially for chronic pain, insomnia, or depression that hasn’t responded to other treatments.
What Elavil (Amitriptyline) Actually Does
Elavil is a tricyclic antidepressant (TCA). It works by increasing levels of serotonin and norepinephrine in the brain - two chemicals that help regulate mood, pain signals, and sleep. But unlike newer SSRIs, it doesn’t pick and choose. It hits multiple receptors at once, which is why it’s effective for more than just depression.
Doctors in the UK often prescribe it off-label for:
- Chronic nerve pain (like diabetic neuropathy or fibromyalgia)
- Chronic tension headaches and migraines
- Insomnia, especially when linked to depression or pain
- Overactive bladder in older adults
It’s not a quick fix. Most people start seeing benefits after 2-4 weeks, and full effects can take 6-8 weeks. Doses for pain are usually lower than for depression - often 10-50 mg at night - which helps reduce side effects.
Why People Look for Alternatives
Despite its effectiveness, Elavil comes with a long list of common side effects:
- Drowsiness (can be useful at night, but dangerous if you drive or operate machinery)
- Dry mouth (can lead to dental problems over time)
- Constipation
- Weight gain (up to 5-10 kg in some patients over 6 months)
- Blurred vision
- Low blood pressure when standing up
- Increased heart rate or irregular heartbeat (riskier in older adults or those with heart conditions)
Because of this, many patients stop taking it - sometimes without telling their doctor. Others try to switch because they’re on multiple medications and want to avoid drug interactions. Elavil can interact with other antidepressants, painkillers, antihistamines, and even some herbal supplements like St. John’s Wort.
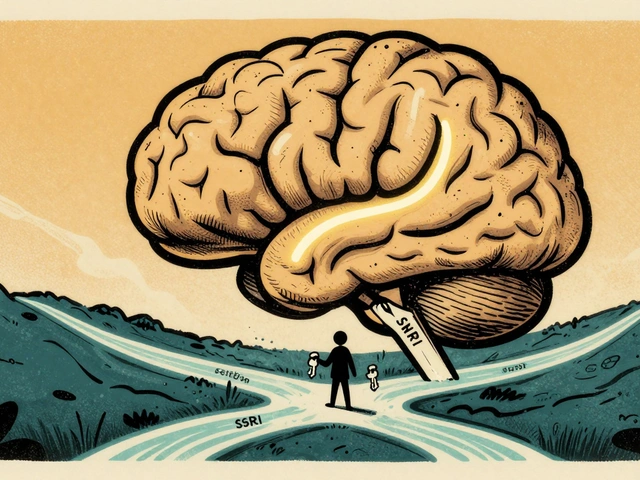
Alternative 1: Duloxetine (Cymbalta)
Duloxetine is an SNRI - a serotonin-norepinephrine reuptake inhibitor - and one of the most common replacements for Elavil in pain management. It’s approved for diabetic neuropathy, fibromyalgia, and chronic musculoskeletal pain. It’s also used for depression and anxiety.
Compared to Elavil:
- Less drowsiness - better for daytime use
- Less weight gain - studies show average weight change is neutral or slight loss
- Lower risk of heart rhythm issues
- More expensive (not always available on NHS prescription without prior authorisation)
- Can cause nausea, especially at first
- May increase blood pressure in some people
Many patients who couldn’t tolerate Elavil’s dry mouth or sedation find duloxetine easier to stick with. But it’s not magic - about 30% of people still experience side effects that lead them to stop.
Alternative 2: Pregabalin (Lyrica)
Pregabalin was originally developed as an antiseizure drug but is now widely used for nerve pain. It’s often prescribed for fibromyalgia, sciatica, and post-herpetic neuralgia.
How it stacks up against Elavil:
- Faster relief - some feel better within days
- Less impact on mood - doesn’t treat depression directly
- Common side effects: dizziness, swelling in hands/feet, weight gain (similar to Elavil), brain fog
- Risk of dependence - some people develop tolerance and need higher doses
- Not recommended for people with kidney problems
Unlike Elavil, pregabalin doesn’t help with sleep or low mood. But if your main problem is sharp, shooting nerve pain, it can be more effective. Many GPs in the UK now try pregabalin first for neuropathic pain, especially in younger patients.
Alternative 3: Mirtazapine (Remeron)
Mirtazapine is an atypical antidepressant that works differently from both TCAs and SSRIs. It boosts serotonin and norepinephrine by blocking certain receptors - and it’s one of the most sedating antidepressants on the market.
Why it’s a strong alternative to Elavil for sleep and depression:
- Very effective for insomnia - often taken at night
- Less dry mouth and constipation than Elavil
- Strong appetite stimulation - helpful for patients who’ve lost weight due to depression
- Weight gain is common (sometimes more than Elavil)
- Can cause dizziness and increased cholesterol in long-term use
It’s not great for pain, though. If you’re on Elavil for both depression and back pain, mirtazapine might help the mood but leave the pain untouched.
Alternative 4: SSRIs like Sertraline or Citalopram
SSRIs (selective serotonin reuptake inhibitors) are the first-line treatment for depression today. Sertraline and citalopram are cheap, widely available, and have fewer side effects than Elavil.
But here’s the catch: they’re not as good for pain. Studies show SSRIs help mild nerve pain slightly, but nowhere near as well as TCAs or SNRIs.
They’re best for:
- Depression or anxiety without chronic pain
- Patients who had bad reactions to Elavil’s anticholinergic effects
- Younger adults who need to stay alert during the day
Side effects like nausea, sexual dysfunction, or insomnia can be worse than Elavil’s drowsiness - especially in the first few weeks. But they’re rarely dangerous, and most people adjust over time.
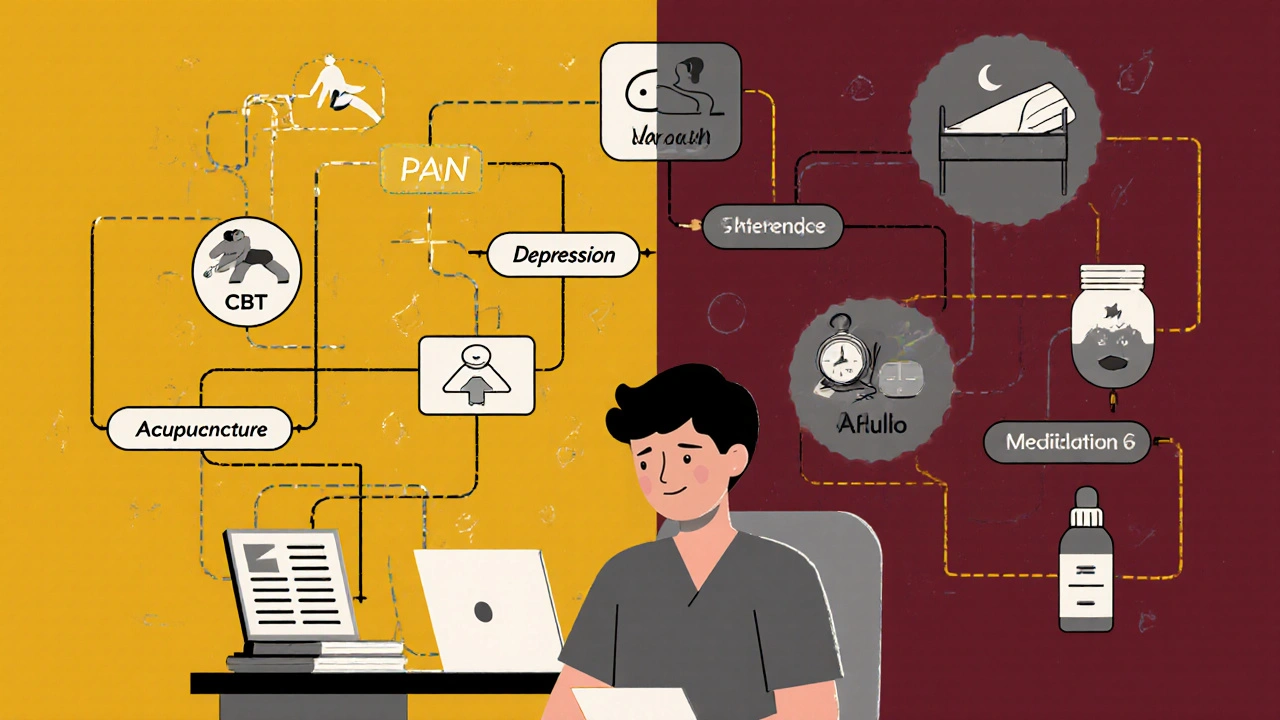
Alternative 5: Non-Drug Options
Before switching medications, many patients don’t realise that non-drug approaches can work as well - or better - than Elavil for certain conditions.
For chronic pain:
- Cognitive behavioural therapy (CBT) - proven to reduce pain perception and improve coping
- Physical therapy and graded exercise - especially for fibromyalgia and lower back pain
- Acupuncture - NHS trials show moderate benefit for headaches and osteoarthritis
For insomnia:
- Sleep hygiene - consistent bedtime, no screens before bed, cool dark room
- Cognitive behavioural therapy for insomnia (CBT-I) - more effective long-term than any sleeping pill
For depression:
- Regular aerobic exercise - 30 minutes, 5 days a week, matches SSRI effectiveness in mild to moderate cases
- Light therapy - especially helpful in winter months in the UK
These aren’t quick fixes, but they don’t come with dry mouth or heart risks. Many patients combine them with lower-dose meds for better results.

Who Should Stay on Elavil?
Not everyone needs to switch. Elavil still has a place - especially for:
- Older adults with chronic pain and depression who’ve tried everything else
- Patients on tight budgets - it’s one of the cheapest antidepressants available
- Those who respond well to it and tolerate side effects
- People with insomnia tied to pain - it’s one of the few drugs that tackles both at once
If you’ve been on Elavil for 6 months or more and feel better, with manageable side effects, there’s no rush to change. But if you’re struggling with drowsiness, weight gain, or constipation, it’s worth exploring alternatives.
How to Talk to Your Doctor About Switching
Never stop Elavil cold turkey. Withdrawal can cause nausea, headaches, anxiety, and even electric-shock sensations. Tapering down over 2-4 weeks is essential.
When you talk to your GP or pharmacist:
- Be specific: "I’m having trouble with dry mouth and weight gain. Can we look at alternatives?"
- Ask: "Is my main issue depression, pain, or sleep? That helps pick the right replacement."
- Request a trial: "Can we try duloxetine for 6 weeks and see if my pain improves?"
- Ask about cost: "Is this available on NHS? If not, how much will it cost out of pocket?"
- Discuss non-drug options: "Would CBT or physiotherapy help alongside medication?"
Doctors are more open to switching than they used to be. Many now see Elavil as a second- or third-line option, especially for younger patients.
What Works Best for You?
There’s no universal winner. The right alternative depends on your biggest problem:
- Pain first? Try duloxetine or pregabalin.
- Sleep and mood? Mirtazapine might be better.
- Just depression? Sertraline or citalopram are safer long-term.
- Want to avoid meds? CBT, exercise, and sleep therapy are proven.
And remember: what works for someone else might not work for you. Many people try 2-3 different drugs before finding the right fit. It’s not failure - it’s part of the process.
Is Elavil still prescribed in the UK?
Yes, Elavil (amitriptyline) is still prescribed in the UK, but less often as a first choice. It’s mainly used for chronic pain, insomnia linked to depression, or when newer antidepressants haven’t worked. The NHS lists it as a cost-effective option, especially for older patients.
Can I switch from Elavil to an SSRI like sertraline?
You can, but only under medical supervision. Switching directly can cause withdrawal symptoms or serotonin syndrome. Your doctor will likely taper your Elavil slowly over 2-4 weeks before starting sertraline. If you’re using Elavil for pain, sertraline may not help as much - so this switch works best if depression is your main issue.
Which is better for nerve pain: amitriptyline or pregabalin?
Both work, but studies show pregabalin often works faster and has fewer cognitive side effects. However, amitriptyline is more effective for patients who also have depression or insomnia. Pregabalin carries a higher risk of dependence and swelling, while amitriptyline can cause dry mouth and heart rhythm changes. Many doctors start with pregabalin in younger patients and amitriptyline in older ones.
Does amitriptyline cause weight gain?
Yes, weight gain is common. Studies show people taking amitriptyline gain an average of 2-5 kg over 6 months, with some gaining more. It’s due to increased appetite and slowed metabolism. Mirtazapine causes similar or worse weight gain. Duloxetine and SSRIs are less likely to cause this side effect.
Are there natural alternatives to Elavil for sleep and pain?
Yes. For sleep, cognitive behavioural therapy for insomnia (CBT-I) is more effective long-term than any sleeping pill. For pain, regular aerobic exercise, physiotherapy, and acupuncture have strong evidence. Magnesium supplements and low-dose melatonin may help some people, but they’re not replacements for prescription meds in moderate to severe cases. Always talk to your doctor before stopping medication.
What to Do Next
If you’re on Elavil and happy with it - keep going. If you’re struggling with side effects or it’s not working well enough, talk to your doctor. Bring a list of your symptoms, what’s bothering you most, and what you’d like to change.
There’s no shame in trying something else. Medicine isn’t one-size-fits-all. The goal isn’t to find the "best" drug - it’s to find the one that lets you live better, with fewer side effects and more energy.

Marshall Washick
November 3, 2025 AT 13:44I’ve been on amitriptyline for 3 years for fibromyalgia and chronic insomnia. It’s not perfect-dry mouth is brutal, and I gained 12 lbs-but it’s the only thing that lets me sleep through the night without relying on benzos. I tried duloxetine, but my pain flared up worse than before. Mirtazapine made me so hungry I was eating peanut butter out of the jar at 2 a.m. Sometimes the old stuff works because it hits the right buttons, even if it’s messy.
My doctor finally lowered my dose to 25mg at night. That’s when things clicked. Less fog, less weight gain, still sleeps me right. Don’t write off TCAs just because they’re old. They’re like a trusty hammer-clunky, but it drives the nail.
Also, CBT-I changed my life. Not a magic cure, but it stopped my brain from racing at 3 a.m. when the med wore off. Combine it with the med, and you’re golden.
Abha Nakra
November 5, 2025 AT 09:26As someone who’s been a nurse for 18 years and worked in pain clinics, I’ve seen this play out a hundred times. Amitriptyline is the OG for neuropathic pain and sleep comorbidity. But you’re right to question it-especially in younger people.
Pregabalin is faster, but the brain fog? Real. I had a patient who couldn’t remember her own kids’ birthdays after 3 months on Lyrica. Duloxetine is great if you can afford it and tolerate the nausea. But for folks on Medicare or Medicaid? Amitriptyline at 10mg is still the only affordable option that works.
And yes, CBT-I is the gold standard for insomnia. No drug beats it long-term. But if you’re too exhausted to even try sleep hygiene? Sometimes you need the med to get to the point where you can do the work. It’s not either/or-it’s both/and.
Tatiana Mathis
November 6, 2025 AT 15:53Thank you for writing this with such clarity. It’s rare to see a medical post that doesn’t sound like a pharmaceutical ad or a fear-mongering rant.
I’m a 52-year-old with diabetic neuropathy and treatment-resistant depression. I was on 75mg of amitriptyline for 4 years. The weight gain was awful-I went from 140 to 185. But the pain? Gone. The depression? Mostly managed.
I switched to duloxetine last year. Pain is 70% better, mood is stable, and I’ve lost 20 lbs. No dry mouth. No constipation. But I get dizzy if I stand too fast, and my anxiety spiked for the first 3 weeks.
My point? There’s no ‘best’ drug. There’s only ‘best for you right now.’ And that changes. I’m considering adding CBT-I next. I’ve started walking 30 minutes daily. I’m not cured, but I’m living again. That’s what matters.
Also, never stop TCAs cold turkey. I saw someone go into withdrawal and think they were having a stroke. It’s terrifying. Taper slow. Talk to your pharmacist. They’re the unsung heroes here.
Nishigandha Kanurkar
November 8, 2025 AT 07:18Tamara Kayali Browne
November 9, 2025 AT 23:25Let’s be brutally honest: prescribing amitriptyline in 2025 is medical malpractice disguised as cost-efficiency. The side effect profile is a laundry list of geriatric nightmares. Dry mouth leads to dental decay, constipation leads to bowel obstructions, anticholinergic burden increases dementia risk. This isn’t ‘old-school medicine’-it’s outdated, dangerous, and lazy.
Duloxetine is not just ‘more expensive’-it’s clinically superior. Pregabalin has risks, yes, but so does prescribing a drug that’s been linked to QT prolongation in 1 in 500 patients over 65.
And CBT? Of course it works. But if you’re too depressed to get out of bed, telling someone to ‘just do CBT’ is like telling a drowning person to ‘just swim.’ You need the life preserver first. But that preserver shouldn’t be a 1960s relic.
This post reads like a pharmaceutical pamphlet from a time when patients had no voice. We deserve better.
Cornelle Camberos
November 10, 2025 AT 14:45It is my solemn duty to inform you that the continued prescription of tricyclic antidepressants constitutes a systemic failure of modern pharmacological oversight. The pharmacokinetic profile of amitriptyline is archaic, its receptor binding affinity is non-selective, and its therapeutic index is dangerously narrow. The fact that it remains on formularies is a testament to institutional inertia, not clinical efficacy.
Furthermore, the assertion that ‘it works for some’ is an epistemological fallacy. Anecdotal success does not constitute evidence-based practice. The NICE guidelines, updated in 2023, explicitly recommend against first-line use of TCAs for any indication except in palliative care.
One must ask: why are we still debating this? The alternatives are not merely ‘options’-they are the standard. To defend amitriptyline is to defend obsolescence. The patient’s suffering is not a justification for outdated protocols-it is a call to action.
And regarding CBT-I? It is not a ‘complementary’ therapy. It is the primary intervention for insomnia. The pharmacological approach should be reserved for refractory cases, and even then, with extreme caution.
I urge all practitioners to reevaluate their prescribing habits. The era of the tricyclic is over. The data is unequivocal.
Lori Johnson
November 11, 2025 AT 06:28My mom was on Elavil for 15 years for chronic pain and depression. She loved it-said it made her feel ‘like herself again.’ But she also gained 40 pounds, couldn’t remember her grandkids’ names half the time, and had to use stool softeners daily.
We switched her to mirtazapine. The weight gain was worse, but she slept like a baby and stopped crying at dinner. Then we added CBT and a walking group. She lost 15 lbs. She started knitting again. She talks about her childhood now-something she hadn’t done in years.
It’s not about which drug is ‘better.’ It’s about which version of your life you want to live. One where you’re numb but pain-free? Or one where you’re a little foggy but still feel joy?
My mom didn’t choose the ‘best’ drug. She chose the one that let her be a grandma again. And that’s worth more than any study.
Melissa Delong
November 12, 2025 AT 19:46Michelle Lyons
November 14, 2025 AT 14:13Neal Burton
November 16, 2025 AT 00:45