What Is Gestational Diabetes?
Gestational diabetes, or GDM, is a type of high blood sugar that starts during pregnancy. It usually shows up between weeks 24 and 28, when hormones from the placenta make your body less responsive to insulin. Your pancreas has to work harder-up to three times harder-to keep your blood sugar in check. When it can’t keep up, glucose builds up in your blood. This isn’t something you had before pregnancy, and it typically goes away after birth. But if left unmanaged, it can lead to serious problems for both you and your baby.
Why Managing Blood Sugar Matters
High blood sugar during pregnancy doesn’t just affect you. It crosses the placenta and tells your baby’s pancreas to make more insulin. That extra insulin turns glucose into fat, which can cause your baby to grow too large. Babies weighing over 8 pounds 13 ounces are at higher risk for shoulder injuries during delivery, low blood sugar after birth, and even breathing problems. You’re also more likely to develop preeclampsia, need a C-section, or go into early labor.
The good news? When blood sugar stays within target ranges, your chances of a healthy birth are nearly the same as someone without gestational diabetes. Studies show that women who stick to their plan reduce the risk of large babies by up to 60% and cut NICU admissions by more than half.
What Your Blood Sugar Targets Should Be
There’s no guesswork here. Doctors use clear, science-backed numbers to guide your daily routine:
- Fasting or before meals: Below 95 mg/dL (5.3 mmol/L)
- One hour after eating: Below 140 mg/dL (7.8 mmol/L)
- Two hours after eating: Below 120 mg/dL (6.7 mmol/L)
These aren’t suggestions-they’re goals. Most women check their blood sugar four to six times a day: first thing in the morning, and one or two hours after each meal. Keeping a log helps spot patterns. If your fasting numbers are high, it might mean you need a bedtime snack with protein and a little carb. If your post-lunch levels spike, you might need to adjust what you ate or when you moved after eating.
Diet: The First Line of Defense
For 70 to 85% of women, diet and movement alone bring blood sugar under control. You don’t need to cut carbs completely-you need to manage them smartly.
Here’s how:
- Carbs: 35-40% of your daily calories. Aim for 45 grams per meal and 15-30 grams per snack. That’s about one cup of cooked rice or two slices of whole grain bread per meal.
- Protein: 20%. Include lean meat, eggs, tofu, or Greek yogurt at every meal to slow sugar absorption.
- Fats: 40%. Healthy fats from avocado, nuts, olive oil, and fatty fish help stabilize glucose.
One simple trick that works for most women: eat protein first, then vegetables, then carbs. A UCSF Health survey found this order lowers post-meal spikes by 25-40 mg/dL. Instead of starting with toast, have scrambled eggs and spinach first, then add the toast.
Portion control matters more than you think. One apple has about 15 grams of carbs. Pair it with a tablespoon of peanut butter, and the spike drops by 30%. That’s the power of combining foods.

Exercise: Move After Meals
Physical activity is one of the most effective, free tools you have. Walking for 30 minutes after meals can drop your blood sugar by 20-30 mg/dL. You don’t need to run a marathon-just get moving.
Brisk walking, swimming, or prenatal yoga five days a week is ideal. Many women find that a 15-minute walk after dinner helps bring down nighttime fasting levels. One Reddit user shared that her fasting numbers dropped 15-25 mg/dL just by walking after breakfast. That’s the kind of change that adds up.
If you’re new to exercise, start slow. Even 10 minutes after each meal helps. The key is consistency, not intensity.
When You Need More Than Diet and Exercise
Even with perfect habits, about 15-30% of women still need medication. That doesn’t mean you failed. It just means your body needed a little extra help.
Insulin is the most common treatment. It’s safe during pregnancy and doesn’t cross the placenta. Many women worry about shots, but most find they get used to them quickly. Modern pens are tiny and nearly painless.
Metformin is sometimes used, especially in places where insulin isn’t easily accessible. But studies show about 30% of women on metformin still need insulin later. It’s not a replacement-it’s a temporary bridge.
Your care team will monitor your progress weekly at first. If your numbers stay high after two weeks of diet and exercise, they’ll talk to you about medication. There’s no shame in it. The goal is a healthy baby, not avoiding pills.
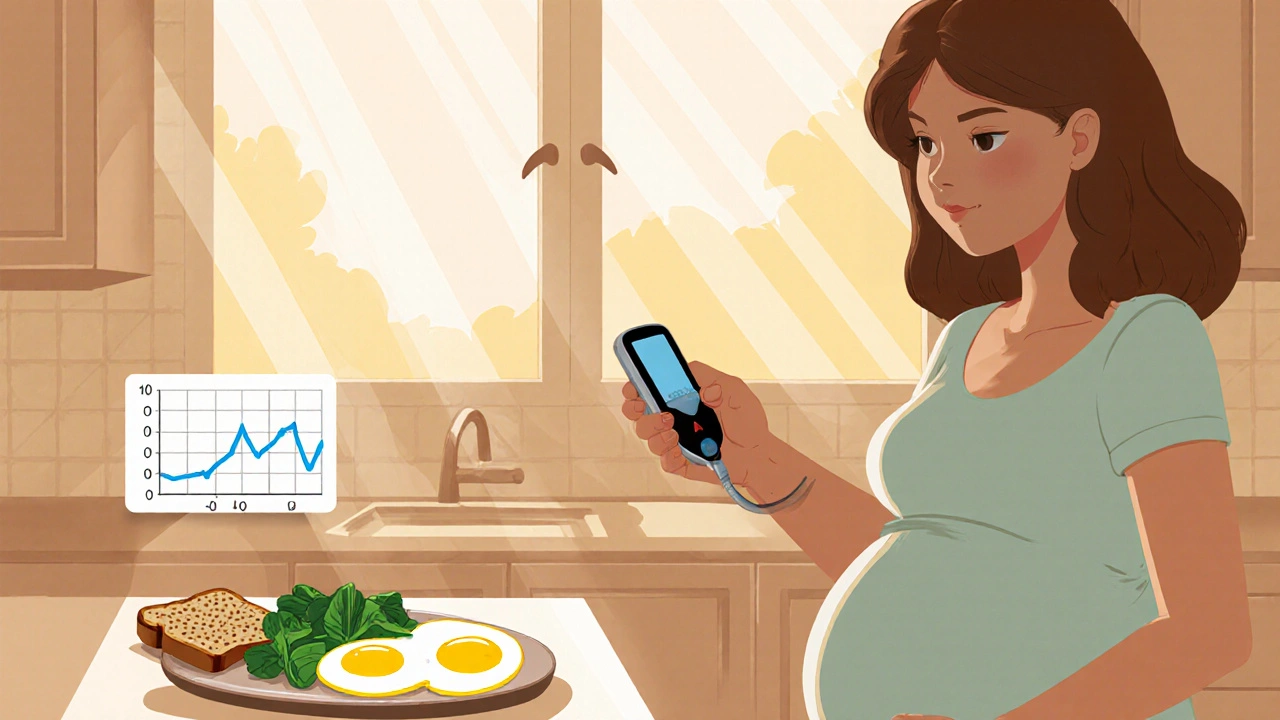
Monitoring: The Daily Habit That Saves Lives
Checking your blood sugar isn’t optional. It’s your compass. Without it, you’re flying blind.
Use a reliable glucose meter and calibrate it daily with control solution. Record each reading with what you ate and when you moved. Look for patterns: Do your numbers spike after rice? Drop after a walk? Rise in the morning? That data tells your doctor what to adjust.
Some women use continuous glucose monitors (CGMs), especially if they had Type 1 diabetes before pregnancy. CGMs show real-time trends and reduce the risk of large babies by 39%. They’re not yet standard for all GDM cases, but adoption is growing fast.
Women who check less than four times a day are over twice as likely to have babies needing NICU care. That’s not a statistic-it’s a warning.

What Happens After the Baby Is Born
Most women’s blood sugar returns to normal within weeks after delivery. But here’s the catch: half of them will develop Type 2 diabetes within 10 years if they don’t take action.
That’s why you need a follow-up test-6 to 12 weeks after birth. You’ll take a 75-gram glucose tolerance test. If your fasting level is above 126 mg/dL or your two-hour level is above 200 mg/dL, you have diabetes. If it’s between those numbers, you have prediabetes.
The next step? Lifestyle. Losing just 5-7% of your body weight after pregnancy cuts your risk of Type 2 diabetes by 58%. That’s not a miracle-it’s math. Eat well. Move daily. Sleep enough. Keep checking your numbers every two years.
Real Stories, Real Results
One woman in Brighton, 34 weeks pregnant, started checking her sugar after meals and noticed her numbers spiked after oatmeal. She switched to a veggie omelet with a small portion of quinoa. Her post-meal levels dropped 40 mg/dL. She didn’t need insulin.
Another woman, terrified of insulin, started walking after dinner. Her fasting levels fell from 110 to 85 mg/dL in three weeks. She said it gave her back control.
On the flip side, women who waited until 30 weeks to get tested or skipped checks often ended up with bigger babies and longer hospital stays. The difference wasn’t luck-it was action.
Where to Find Help
You don’t have to figure this out alone. Certified Diabetes Care and Education Specialists (CDCES) are trained to walk you through carb counting, meter use, and meal planning. Most hospitals offer a one-time 1-2 hour session right after diagnosis.
Resources like the American Diabetes Association’s Healthy Eating for Pregnancy guide and the CDC’s postpartum transition plan are free and easy to follow. Online communities like DiabetesSisters and Reddit’s r/GestationalDiabetes offer real talk from women who’ve been there.
If your care team gives you conflicting advice-say, your OB says eat more carbs and your endocrinologist says cut them-ask for a joint consultation. Consistency saves lives.
Final Thought: This Is Temporary, But the Habits Last
Gestational diabetes lasts only nine months. But the habits you build now-eating balanced meals, moving daily, checking your numbers, listening to your body-last a lifetime. You’re not just protecting your baby today. You’re protecting yourself for decades to come.
It’s not about perfection. It’s about progress. One meal at a time. One walk at a time. One check at a time.
Can gestational diabetes go away before delivery?
Yes, it’s possible. Some women bring their blood sugar under control with diet and exercise alone and never need medication. But even if your numbers normalize, you still need to keep monitoring until delivery. The condition can return quickly if you change your routine. The goal isn’t to make it disappear-it’s to keep it managed.
Will my baby have diabetes because of gestational diabetes?
Not directly. Your baby won’t be born with diabetes. But they are at higher risk for obesity and Type 2 diabetes later in life, especially if they were large at birth or if you don’t make healthy changes after pregnancy. The good news? Breastfeeding and a healthy diet for your child can significantly lower that risk.
Can I eat fruit with gestational diabetes?
Absolutely. Fruit is full of fiber, vitamins, and antioxidants. But portion and timing matter. One small apple, half a banana, or three-quarters of a cup of berries counts as one carb choice (15g). Eat fruit with a source of protein or fat-like a handful of almonds or a spoon of Greek yogurt-to slow the sugar spike. Avoid fruit juice entirely-it’s sugar without fiber.
Do I need to avoid all sugar?
No. You don’t need to cut out sugar entirely. But you need to be smart about it. Natural sugars in fruit and dairy are fine in controlled portions. Added sugars-like in cookies, soda, candy, or sweetened yogurt-should be avoided. They cause rapid spikes and offer no nutrition. Read labels. If sugar is one of the first three ingredients, skip it.
Is gestational diabetes my fault?
No. It’s not caused by eating too much sugar or being lazy. It’s caused by hormonal changes during pregnancy that affect how your body uses insulin. Genetics, age, weight, and family history play roles-but no one chooses to get it. Blaming yourself only adds stress, which can make blood sugar harder to control. Focus on what you can do today, not guilt about the past.
Can I still have a vaginal birth with gestational diabetes?
Yes, absolutely. Many women with GDM have vaginal deliveries. The key is keeping your baby’s size in check. If your baby is growing too large, your provider may suggest induction or a C-section. But if your blood sugar is well-managed, your chances of a vaginal birth are just as high as someone without GDM. Talk to your provider early about your birth plan.
What if I don’t follow the diet?
It’s not about being perfect-it’s about consistency. Missing a day won’t ruin everything. But if you consistently eat large portions of refined carbs, skip movement, or skip checks, your baby’s risk of complications increases. The goal isn’t to be flawless-it’s to make better choices more often than not. Every small change adds up.
How often should I see my doctor?
After diagnosis, you’ll typically see your provider weekly for the first month, then every two weeks until delivery. If you’re on insulin or your numbers are hard to control, you may need more frequent visits. Your care team will adjust based on your progress. Don’t skip appointments-even if you feel fine. Your numbers tell the real story.
Can I breastfeed if I had gestational diabetes?
Yes, and you should. Breastfeeding helps your body return to normal insulin sensitivity faster. It also lowers your baby’s risk of obesity and Type 2 diabetes later in life. You might feel hungrier while nursing, so keep healthy snacks nearby-nuts, cheese, yogurt, or whole grain crackers with hummus. Stay hydrated and eat balanced meals. Your body needs fuel, and breastfeeding is hard work.
What’s the biggest mistake women make with gestational diabetes?
Waiting too long to act. Many women ignore early symptoms like extreme thirst, frequent urination, or fatigue, thinking it’s just pregnancy. Others skip glucose tests because they’re scared of the results. The biggest risk isn’t the diagnosis-it’s delay. The earlier you start managing, the better your outcome. Don’t wait for a crisis to take action.

Christopher K
November 20, 2025 AT 05:11harenee hanapi
November 21, 2025 AT 18:07Christopher Robinson
November 22, 2025 AT 14:00James Ó Nuanáin
November 22, 2025 AT 20:48Nick Lesieur
November 24, 2025 AT 19:02Andy Feltus
November 25, 2025 AT 15:49river weiss
November 26, 2025 AT 07:46Brian Rono
November 27, 2025 AT 03:52seamus moginie
November 28, 2025 AT 17:15Dana Dolan
November 29, 2025 AT 22:40Steve and Charlie Maidment
December 1, 2025 AT 08:31Michael Petesch
December 1, 2025 AT 19:32Richard Risemberg
December 2, 2025 AT 16:49Andrew Montandon
December 4, 2025 AT 06:19Sam Reicks
December 4, 2025 AT 09:09