When your body makes too much antidiuretic hormone, a hormone that tells your kidneys to hold onto water. Also known as vasopressin, it can cause your blood sodium to drop dangerously low — a condition called hyponatremia. This is the core problem behind SIADH, the Syndrome of Inappropriate Antidiuretic Hormone Secretion. It’s not a disease on its own, but a side effect of other issues — like lung infections, brain injuries, or certain cancer treatments. And when it happens, you need the right SIADH meds, drugs designed to block or reduce the effects of excess antidiuretic hormone to bring sodium back to safe levels.
Not all SIADH meds work the same way. Some, like tolvaptan, a vasopressin receptor antagonist, stop the hormone from acting on your kidneys so your body can flush out extra water. Others, like demeclocycline, an antibiotic that makes kidneys less responsive to ADH, work slowly but are cheaper and used for long-term cases. Then there’s fluid restriction — not a drug, but often the first step. Some doctors still use lithium or chlorpropamide, though those come with serious risks. The choice depends on how fast your sodium dropped, how sick you are, and what’s causing the SIADH in the first place. You can’t just pick one and hope for the best — wrong meds or wrong doses can make things worse.
What you’ll find in the posts below isn’t a list of every drug ever tried for SIADH. It’s a practical guide to what’s actually used today, how they compare, and what to watch out for. You’ll see how drugs like amitriptyline — yes, an antidepressant — can accidentally trigger SIADH, and why some medications used for pain or depression might need to be swapped out. You’ll also find real-world advice on monitoring sodium levels, avoiding dangerous interactions, and knowing when to switch treatments. These aren’t theoretical discussions. They’re based on what patients and doctors have seen work — or fail — in real cases. Whether you’re managing SIADH yourself or helping someone who is, this collection gives you the clear, no-fluff facts you need to make smarter choices.

Natrise (tolvaptan) raises sodium levels fast but carries liver risks and high costs. Learn how fluid restriction, urea, demeclocycline, and salt tablets compare as safer, cheaper alternatives for hyponatremia.

Explore how liver failure impacts vision, from jaundice and dry eye to retinal hemorrhages, and learn practical steps to protect eye health while managing liver disease.
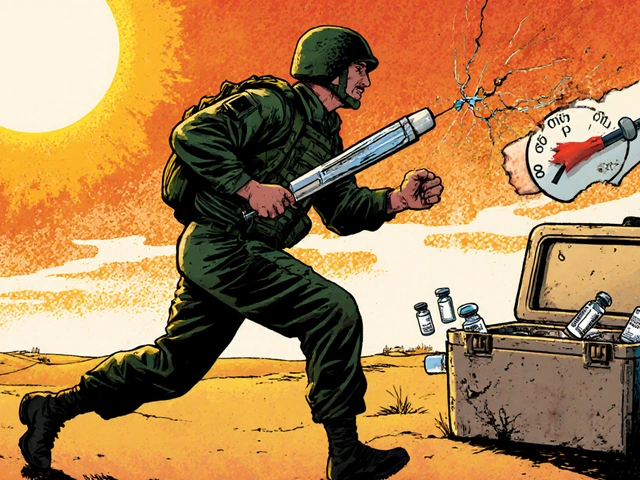
Military deployment exposes medications to extreme heat, storage failures, and access delays that can render life-saving drugs ineffective. From vaccines to insulin, improper storage threatens soldier readiness-and the military is racing to fix it.

A detailed side‑by‑side comparison of Neoral (Cyclosporine) with Tacrolimus, Sirolimus, Mycophenolate, and Azathioprine, covering mechanisms, dosing, side effects, cost and monitoring.

Learn how drug take-back programs safely dispose of unused medications through permanent drop boxes, mail-back envelopes, and nationwide events. Find out what you can and can’t dispose of, and how to locate the nearest collection site.

Understand how 2025 Medicare Part D formulary updates are forcing generic and biosimilar switches, what drugs are affected, and how to protect your coverage before January 1.