Hyperkalemia Risk Calculator
What to do next:
- Recommended Get a baseline potassium test before starting trimethoprim
- Recommended Monitor potassium levels at 48-72 hours
- Recommended Discuss safer antibiotic alternatives with your doctor
- Critical Contact your doctor immediately if you experience muscle weakness, irregular heartbeat, or nausea
When you take an antibiotic like Bactrim or Septra for a urinary tract infection, you probably don’t think about your potassium levels. But for some people, especially older adults or those on blood pressure meds, this common drug can push potassium dangerously high - fast. And that’s not just a lab number. High potassium can stop your heart.
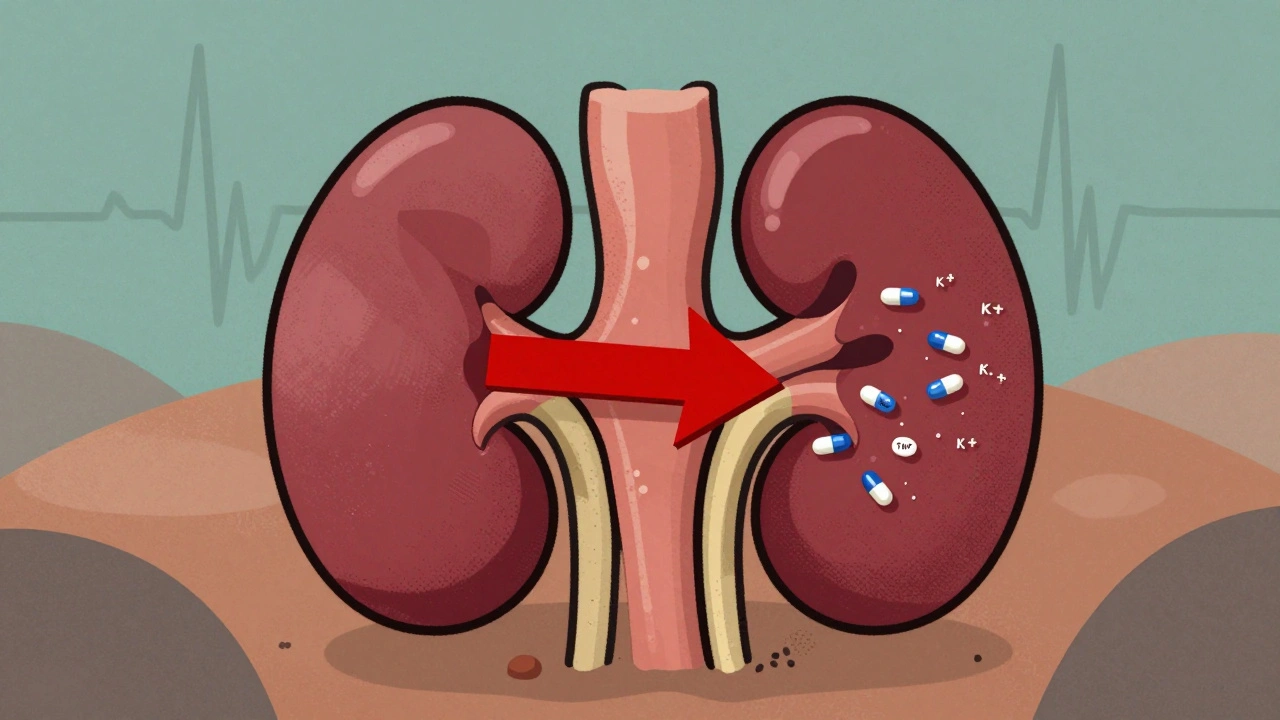
How Trimethoprim Raises Potassium
Trimethoprim, the antibiotic part of TMP-SMX, doesn’t work like most antibiotics. It acts like a hidden diuretic - but not the kind that makes you pee more. Instead, it blocks the same channel in your kidneys that amiloride, a potassium-sparing diuretic, does. This channel, called ENaC, helps your body get rid of potassium by letting sodium back in. When trimethoprim blocks it, sodium doesn’t get reabsorbed, and potassium stays trapped in your blood.This isn’t a slow, gradual effect. Studies show potassium levels can jump by 0.5 to 1.5 mmol/L within just 48 to 72 hours of starting the drug. In one case, an 80-year-old woman with normal kidney function took a single daily dose of Bactrim for pneumonia prevention - and three days later, her potassium hit 7.8 mmol/L. Normal is 3.5 to 5.0. She had cardiac arrest.
The reason this happens so quickly? Trimethoprim concentrates in the kidneys at levels 10 to 50 times higher than in your blood. Even a low dose - like the 160/800 mg tablet - can cause this. It doesn’t matter if your kidneys look fine on paper. The drug doesn’t care. It goes straight to the tubules and starts blocking channels.
Who’s at the Highest Risk?
Not everyone gets hyperkalemia from trimethoprim. But certain people are sitting on a time bomb.- People over 65 - age reduces kidney function, even if creatinine looks normal.
- Those on ACE inhibitors or ARBs (like lisinopril, losartan) - these drugs already reduce potassium excretion. Add trimethoprim, and you get a double hit.
- People with chronic kidney disease (eGFR under 60) - their kidneys can’t clear trimethoprim well, so levels build up.
- Diabetics - often have kidney changes and are on ACEIs/ARBs.
- Those already taking potassium-sparing diuretics like spironolactone.
A 2020 study found that if you’re over 65, have diabetes, CKD stage 3 or worse, and are on an ACEI or ARB - your chance of developing dangerous hyperkalemia on trimethoprim jumps to 32%. That’s one in three. Compare that to 4.3% in people taking other antibiotics.
How Much Higher Is the Risk?
Let’s put this in perspective. A major 2014 study tracked over 4,000 hospital admissions for hyperkalemia. Among older adults on blood pressure meds:- Those taking TMP-SMX had a 6.7 times higher risk of being hospitalized for high potassium than those taking amoxicillin.
- Nitrofurantoin? No increased risk. It’s safe to use in this group.
- One in every 150 people on TMP-SMX with these risk factors ended up in the hospital because of potassium.
And it’s not just hospital visits. Between 2010 and 2020, the FDA recorded 1,247 cases of trimethoprim-linked hyperkalemia - including 43 deaths. Nearly 70% of those who died were over 65. In one Reddit thread, a doctor wrote: “72-year-old woman on lisinopril. Normal creatinine. Took Bactrim for UTI. Three days later, potassium 6.8. Needed emergency dialysis.”
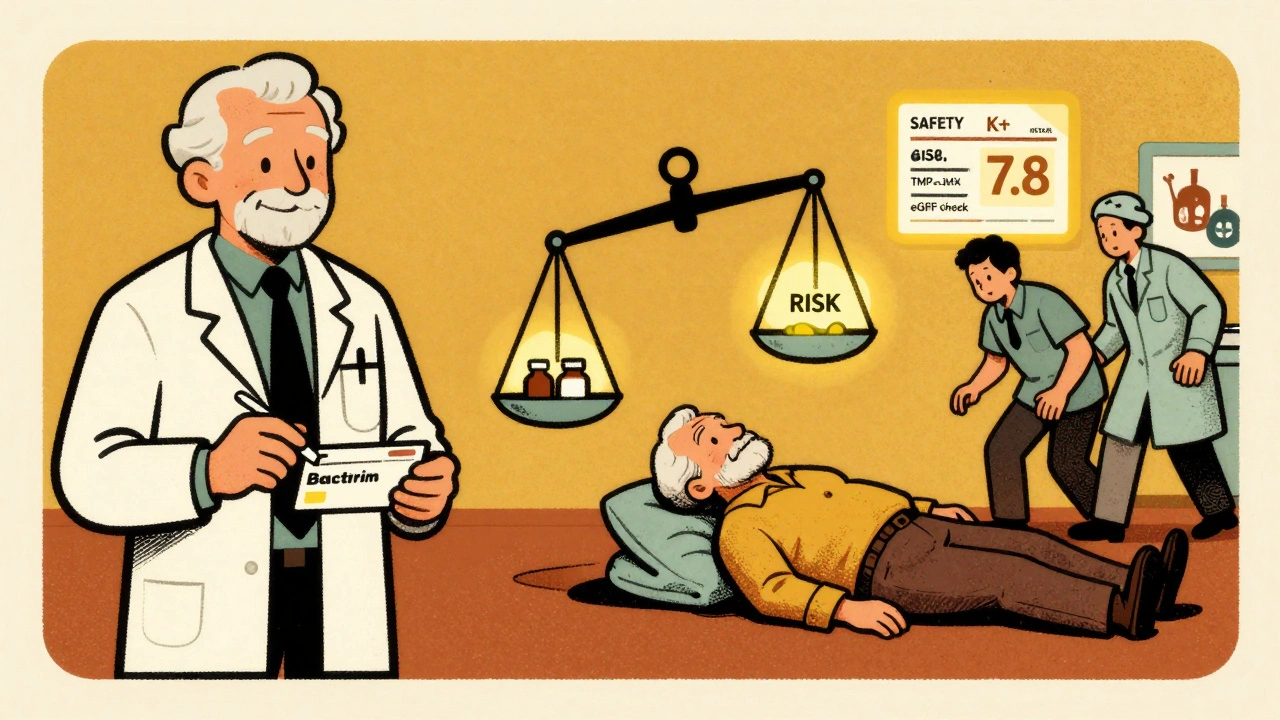
Why Do Doctors Still Prescribe It?
You might wonder - if it’s this dangerous, why is it still on the shelf?Because for some conditions, there’s no better option.
Trimethoprim-sulfamethoxazole is still first-line for Pneumocystis jirovecii pneumonia (PCP) in immunocompromised patients - like those with HIV or on chemotherapy. It’s cheap, effective, and works where other antibiotics fail. The Infectious Diseases Society of America still recommends it for this use.
But here’s the catch: even in these high-risk patients, the risk isn’t zero. It’s managed. That means checking potassium before and during treatment. In fact, studies show that when doctors monitor potassium levels, deaths drop dramatically.
For routine infections - UTIs, sinus infections, ear infections - there are safer alternatives. Nitrofurantoin for UTIs. Amoxicillin for most respiratory infections. Yet, a 2022 analysis found that over 14 million TMP-SMX prescriptions are written each year in the U.S. - and nearly 4.2 million go to people over 65.
What Should You Do?
If you’re prescribed trimethoprim-sulfamethoxazole, here’s what you need to know:- Ask if you’re at risk. Are you over 65? On lisinopril, losartan, or similar meds? Have kidney disease or diabetes? If yes, ask: “Is there a safer antibiotic?”
- Get a baseline potassium test. Before you even take the first pill, your doctor should check your potassium. If it’s already above 5.0 mmol/L, don’t start trimethoprim.
- Get tested again in 48-72 hours. That’s when potassium peaks. If it’s above 5.5, stop the drug immediately.
- Know the warning signs. Muscle weakness, irregular heartbeat, nausea, fatigue - these can be early signs of high potassium. Don’t wait for a lab result if you feel off.
- Don’t assume your kidneys are fine. Creatinine can look normal even if your kidney function is declining. eGFR is the real number to watch.
Some hospitals now have electronic alerts that block TMP-SMX orders if the patient is on an ACEI/ARB and hasn’t had a recent potassium test. One study showed this cut hyperkalemia cases by over half. But in most clinics? No alert. No check. Just a prescription.
What Are the Alternatives?
For most common infections, you don’t need TMP-SMX.- UTIs: Nitrofurantoin, fosfomycin, or cephalexin are safer choices. Nitrofurantoin has no link to hyperkalemia.
- Sinus or ear infections: Amoxicillin or doxycycline.
- Respiratory infections: Amoxicillin-clavulanate or azithromycin.
- PCP prophylaxis (for immunocompromised): Trimethoprim is still best - but only if potassium is monitored weekly.
There’s no one-size-fits-all. But there’s always a safer option - if you ask.
The Bottom Line
Trimethoprim isn’t evil. It saves lives - especially in people with weakened immune systems. But for the vast majority of patients taking it for a simple infection, the risk of hyperkalemia far outweighs the benefit.It’s not about avoiding antibiotics. It’s about choosing the right one. If you’re on blood pressure meds, over 65, or have kidney issues, don’t let your doctor reach for Bactrim by default. Ask for the alternative. Demand a potassium test. Your heart might depend on it.
Hyperkalemia doesn’t come with a warning siren. It sneaks in quietly. And by the time you feel it, it might be too late.

Richard Eite
December 10, 2025 AT 00:01So let me get this straight - we’re letting doctors prescribe a drug that can kill old folks just because it’s cheap and we’re too lazy to test potassium? This is why American healthcare is a joke.
Jennifer Blandford
December 10, 2025 AT 01:20I had my grandma on Bactrim last year for a UTI and she almost didn’t make it. Her potassium spiked to 6.9. We were lucky they caught it in time. Why isn’t this common knowledge? Everyone should know this before they take it.
Philippa Barraclough
December 10, 2025 AT 17:00The pharmacokinetics of trimethoprim’s renal tubular action are indeed fascinating. The drug’s high concentration gradient in the distal nephron allows for potent ENaC inhibition, effectively mimicking amiloride’s mechanism without the diuretic component. This results in reduced sodium reabsorption and consequent potassium retention, particularly in patients with compromised renal clearance or concomitant RAAS inhibition. The temporal kinetics are alarming - peak serum potassium elevation often occurs within 72 hours, which is why routine monitoring is not merely prudent but mandatory in high-risk cohorts. The 2020 cohort study cited demonstrates a clear dose-response relationship even at prophylactic doses, suggesting that therapeutic intent does not mitigate pharmacological risk. Furthermore, the assumption that normal serum creatinine equates to adequate renal function is archaic; eGFR remains the only reliable indicator of glomerular filtration reserve in elderly populations.
om guru
December 12, 2025 AT 00:06Doctors must act with wisdom. A simple test can save a life. Always check potassium before prescribing. Always. No exceptions. This is medicine with responsibility.
Ronald Ezamaru
December 12, 2025 AT 11:30As a pharmacist, I’ve seen this too many times. Elderly patients on lisinopril get Bactrim for a UTI, come back three days later in cardiac arrest. We have protocols in our hospital now - if you’re over 65 and on an ACEI/ARB, the system flags it and forces a potassium check before dispensing. It’s not perfect, but it’s saved lives. We need this everywhere.
Lola Bchoudi
December 12, 2025 AT 21:02From a clinical pharmacology standpoint, the ENaC blockade by trimethoprim is a textbook example of off-target pharmacodynamic interaction. The drug’s structural similarity to amiloride enables competitive inhibition at the alpha-subunit of the epithelial sodium channel in the collecting duct. This results in decreased luminal sodium reabsorption, which reduces the electrochemical gradient necessary for potassium secretion. The consequence is hyperkalemia, which can be lethal in the context of concomitant RAAS blockade. The 6.7-fold increased hospitalization risk versus amoxicillin is not statistically anomalous - it’s a predictable drug-drug interaction. The real failure is in the lack of clinical decision support integration in EHRs. We have the data. We have the tools. We just don’t enforce them.
Shubham Mathur
December 13, 2025 AT 00:55Look, I’m from India, we don’t have fancy labs everywhere, but even here we know: don’t give Bactrim to old people on blood pressure pills. My uncle died from this. No test. No warning. Just a script. This isn’t science, it’s negligence. We need laws, not just guidelines.
Stacy Tolbert
December 13, 2025 AT 14:31I’m a nurse. I’ve held so many hands while they waited for potassium to come down. I’ve seen the EKGs go flat. I’ve seen families cry. This isn’t just a lab value. It’s someone’s last breath. Why does this keep happening?
Taya Rtichsheva
December 14, 2025 AT 17:51so like... bactrim is just secretly a heart killer? wow. i thought it was just for infections. guess i’ll be asking my doc for nitrofurantoin next time. also, why do they even still sell this? someone’s making bank on old people dying
Morgan Tait
December 15, 2025 AT 13:13Did you know the FDA has known about this since 1998? But Big Pharma lobbied to keep it on the market because it’s dirt cheap. Meanwhile, they’re selling you expensive alternatives. This isn’t an accident. It’s a profit-driven massacre. And they wonder why people don’t trust doctors.
Ryan Brady
December 16, 2025 AT 14:59USA bad. Canada got it right. They banned this for seniors years ago. We’re still playing Russian roulette with antibiotics. 🤡
Darcie Streeter-Oxland
December 17, 2025 AT 01:17It is regrettable that such a well-documented and preventable adverse drug reaction continues to be under-recognized within primary care settings. The absence of mandatory pre-prescription electrolyte assessment constitutes a systemic failure in clinical governance.
Gilbert Lacasandile
December 18, 2025 AT 22:46Yeah, I’ve been on Bactrim before and I’m 70 and on lisinopril. My doc didn’t mention anything. I just got lucky I guess. But now I’m gonna ask next time. Thanks for the heads up.
Tim Tinh
December 20, 2025 AT 17:46my grandma took this for a UTI and i had to rush her to the er. she was so weak and her heart was acting weird. doc said it was the bactrim. now i always check if her meds are safe. you guys need to spread this more. people need to know.
Brianna Black
December 21, 2025 AT 07:23Hyperkalemia induced by trimethoprim is not an incidental finding-it is a predictable, preventable, and clinically significant adverse event. The pharmacological mechanism is unequivocal. The epidemiological data are unequivocal. The mortality rate is unequivocal. The failure to implement mandatory pre-prescription potassium screening in high-risk populations represents a catastrophic breach of the standard of care. Institutions that continue to permit this practice are complicit in patient harm.