When you hear generic drug coverage, the way health plans pay for medications that are chemically identical to brand-name drugs but cost far less. Also known as generic medication reimbursement, it’s the system that lets millions of people afford prescriptions without breaking the bank. This isn’t just about saving a few dollars—it’s about keeping people on their meds. If your blood pressure pill, antidepressant, or diabetes drug isn’t covered, you might skip doses, split pills, or go without. That’s not a choice—it’s a risk.
Generic drug coverage doesn’t happen by accident. It’s shaped by FDA approval, the process that proves a generic version works just like the brand-name drug. Also known as ANDA approval, it’s what lets companies sell cheaper versions without repeating costly clinical trials. Then there’s drug pricing, how manufacturers, insurers, and pharmacies negotiate what gets paid for each pill. Also known as pharmaceutical cost structure, it’s why two identical pills can cost $4 at one pharmacy and $40 at another. And don’t forget insurance coverage, the rules your plan sets about which generics are included, what tier they’re on, and how much you pay out of pocket. Also known as formulary placement, it’s the hidden map that decides if your medicine is affordable or out of reach.
Most plans cover generics first—because they’re cheaper and just as safe. But coverage isn’t guaranteed. Some insurers block certain generics unless you try the brand first. Others limit how many you can get per month. And sometimes, even if a generic is covered, the copay is still too high for people on fixed incomes. That’s where understanding your plan’s formulary matters. It’s not just fine print—it’s your access ticket.
What you’ll find here are real, practical answers. Not theory. Not marketing. Posts that show you how governments keep generic prices low without price caps, why some generics look different but work the same, and how to spot when your coverage is letting you down. You’ll learn how to check if your drug is covered, what to do when it’s not, and how to push back when costs don’t make sense. This isn’t about guessing. It’s about knowing exactly where you stand—and how to fix it.
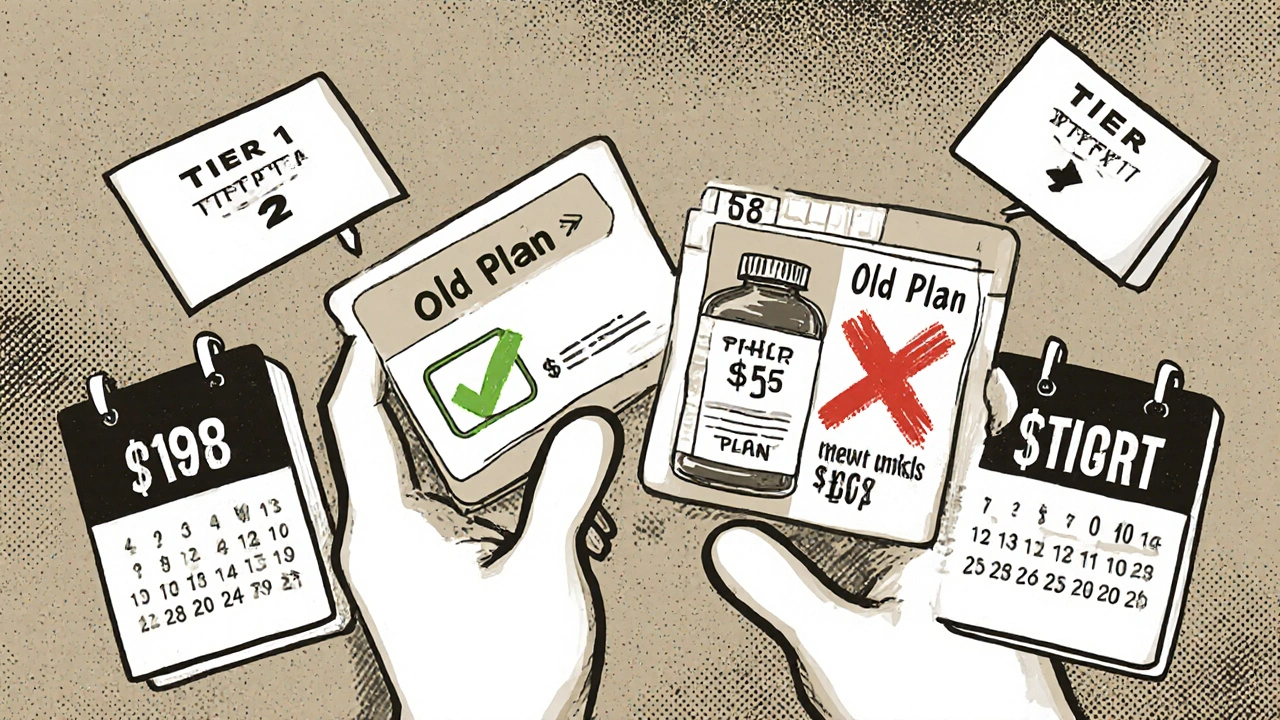
When switching health plans, your generic drug coverage can save or cost you hundreds a year. Learn how formulary tiers, deductibles, and state rules impact your prescription costs-and how to avoid expensive surprises.

Compare Betapace (sotalol) with top anti‑arrhythmic alternatives, covering mechanisms, dosing, side effects, and when to choose each.

Explore how genetics, therapeutic monitoring, and new delivery methods can personalize ethambutol therapy, reduce eye toxicity, and boost TB treatment success.
Ceramides restore the skin barrier in eczema by replacing missing lipids. Proper bathing-short, lukewarm soaks followed by immediate moisturizing-boosts results. Learn how to use ceramides effectively for lasting relief.
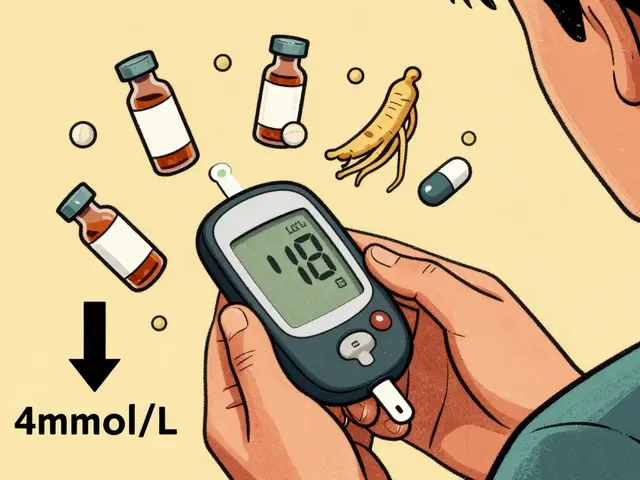
Ginseng may help lower blood sugar in type 2 diabetes, but it can dangerously interact with insulin and oral meds. Learn how to monitor your levels, avoid risks, and use it safely if approved by your doctor.

Learn how to report adverse drug reactions to the FDA's MedWatch program. Understand what counts as reportable, how to fill out the form, and why your report matters for drug safety.