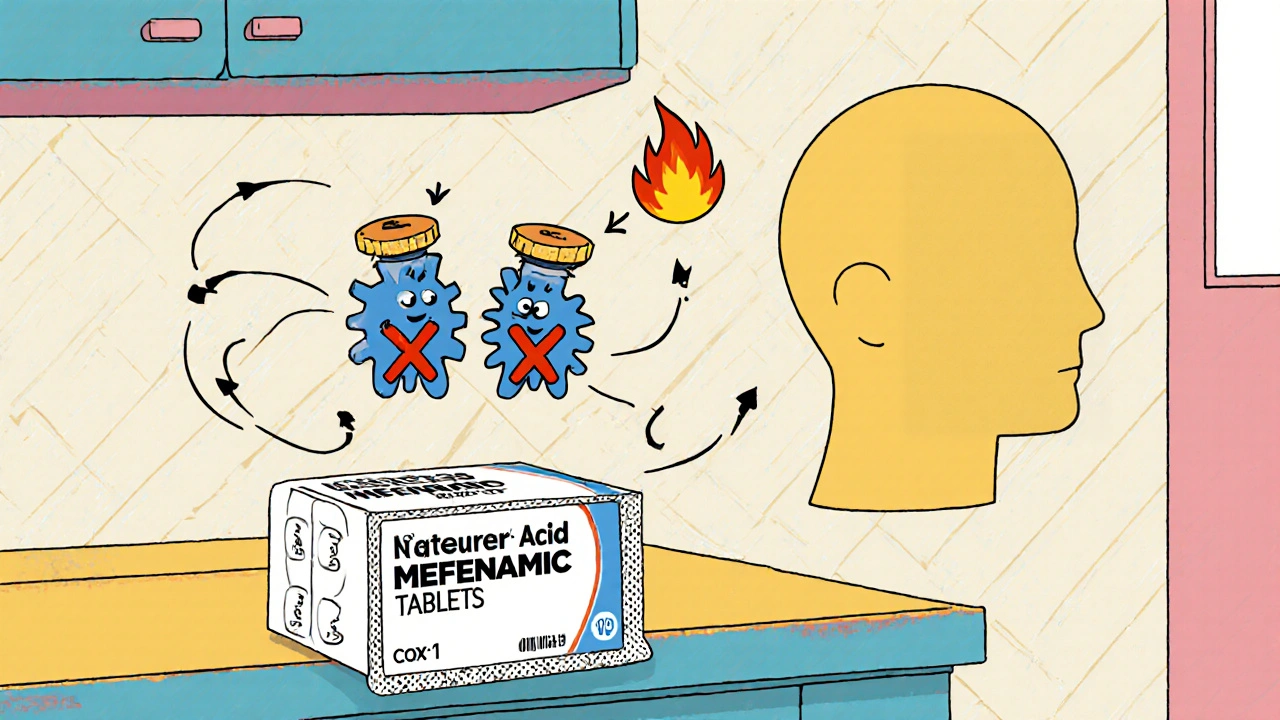
When talking about mefenamic acid side effects, a non‑steroidal anti‑inflammatory drug (NSAID) used for pain and inflammation. Also known as Mefenamic, it works by blocking prostaglandin production, which eases aches but can also trigger unwanted reactions.
One of the biggest companions of mefenamic acid is the broader class of NSAIDs, drugs that reduce pain, fever, and swelling by inhibiting COX enzymes. Like its peers, mefenamic acid can irritate the stomach lining, leading to gastrointestinal bleeding, a serious bleed that may show up as black stools, vomiting blood, or sudden abdominal pain. If you combine the pill with alcohol or take it on an empty stomach, the risk jumps dramatically.
The kidneys act as the body’s filtration system, and they’re sensitive to NSAID exposure. Renal impairment, a condition where the kidneys can’t clear waste efficiently can develop when mefenamic acid reduces blood flow to renal tissue. This effect is especially common in older adults, people with hypertension, or anyone already taking diuretics. In practice, you might notice swelling, reduced urine output, or a rise in blood pressure – all signs that the drug is taxing the kidneys.
Because the drug’s chemistry influences both stomach and kidney health, the relationship can be summed up as: m efenamic acid side effects often involve a trade‑off between pain relief and organ safety. Managing that trade‑off means monitoring lab values, staying hydrated, and avoiding other nephrotoxic agents.
Another thread that ties everything together is drug interactions, instances where two or more medications affect each other's effectiveness or toxicity. When mefenamic acid mixes with anticoagulants like warfarin, the bleeding risk multiplies. Pairing it with other NSAIDs, corticosteroids, or selective serotonin reuptake inhibitors (SSRIs) can also amplify stomach irritation. Even over‑the‑counter supplements such as omega‑3 fatty acids or high‑dose vitamin E may nudge the bleeding odds higher.
In short, the safety profile of mefenamic acid is shaped by three core factors: the drug class (NSAIDs), the organ systems most at risk (GI tract and kidneys), and the other substances you’re taking. Understanding each factor helps you predict which side effects might appear and when.
For patients who need short‑term relief, the best approach is a low dose for the briefest period. Take the pill with food, avoid alcohol, and check in with your clinician if you have a history of ulcers, kidney disease, or are on blood thinners. If you’re already on a regimen that includes multiple NSAIDs or blood‑thinners, ask your doctor whether a different pain reliever—like acetaminophen or a COX‑2 selective agent—might be safer.
From a clinician’s perspective, the decision‑making process follows a simple triple: mefenamic acid requires risk assessment, influences gastrointestinal and renal outcomes, and interacts with common cardiovascular medications. By tracking each link, providers can tailor dosing, schedule lab checks, and offer protective strategies such as proton‑pump inhibitors for high‑risk stomachs.
Below you’ll find a curated collection of articles that dive deeper into each of these areas. Whether you’re curious about how mefenamic acid compares to other NSAIDs, looking for guidance on managing GI bleeding risks, or need tips on spotting early signs of renal trouble, the posts ahead cover practical advice, real‑world examples, and the latest research findings. Dive in to get the full picture and make an informed choice about using mefenamic acid safely.
Explore how mefenamic acid influences bone mineral density, review clinical evidence, compare it with other NSAIDs, and get practical tips for patients and prescribers.

Learn what Rhinocort does, how to spray it correctly, dosage guidelines, common side effects and alternatives for allergy relief.

Switching children to generic medications can save money-but it can also risk their health. Learn why pediatric patients are uniquely vulnerable to changes in drug formulations, how insurance policies drive unsafe switches, and what parents and doctors must do to protect kids on chronic meds.

Learn how to manage salt intake while taking ramipril to lower blood pressure, reduce side effects, and protect your heart and kidneys. Practical diet tips, hidden sodium sources, and what to avoid.

Discover seven effective alternatives to Diclofenac in 2025. Each option is explored in terms of benefits and drawbacks, offering insight into modern pain management methods. Learn the unique features of each alternative, including their impacts on different types of pain and side effects. Whether you're managing chronic pain or seeking a safer medication, this guide provides valuable information for better health decisions.

Compare Waklert (armodafinil) with modafinil, Adrafinil, Adderall, and natural alternatives to find the safest, most effective option for focus and alertness. Learn what works, what doesn’t, and why.