When working with sulfonylurea alternatives, non‑insulin oral agents that lower glucose with a lower hypoglycaemia risk than traditional sulfonylureas. Also known as non‑sulfonylurea hypoglycemics, it gives doctors and patients a broader toolbox for type 2 diabetes management.
One of the most common alternatives is Metformin, a biguanide that improves insulin sensitivity and reduces hepatic glucose production. Metformin forms the backbone of many modern regimens because it is cheap, weight‑neutral and has decades of safety data. GLP‑1 agonists represent a newer class; these injectable or oral drugs mimic the gut hormone GLP‑1, stimulating insulin release only when glucose is high, slowing gastric emptying and often promoting weight loss. Another powerful group is SGLT2 inhibitors, agents that block kidney reabsorption of glucose, sending excess sugar out in the urine. They not only lower HbA1c but also lower blood pressure and protect the heart and kidneys. DPP‑4 inhibitors, drugs that prolong the action of endogenous GLP‑1, provide modest glucose drops with minimal side‑effects sit between the cost‑effective Metformin and the premium GLP‑1 agonists, offering an oral option that’s easy to add to existing therapy.
Choosing the right sulfonylurea alternative depends on three key attributes: efficacy, safety profile, and patient‑specific factors. For a newly diagnosed patient who wants a low‑cost start, Metformin usually takes the lead (efficacy ≈ 1%‑1.5% HbA1c reduction, hypoglycaemia ≈ 0%). If weight loss is a priority, GLP‑1 agonists can shave off several kilograms while dropping HbA1c by up to 2%. Patients with chronic kidney disease may benefit most from SGLT2 inhibitors because they also reduce albuminuria and cardiovascular events. DPP‑4 inhibitors are often chosen when tolerability is paramount; they rarely cause gastrointestinal upset and have a flat hypoglycaemia risk.
Beyond the drug class, the treatment plan requires monitoring renal function, liver enzymes and, for SGLT2 inhibitors, signs of genital infections. Many clinicians pair Metformin with one of the newer agents to achieve synergistic glucose control while keeping side‑effects low. Lifestyle coaching—diet, exercise, weight management—remains a non‑negotiable part of any regimen, regardless of the pharmacologic choice.
Below you’ll find detailed side‑by‑side comparisons, cost breakdowns, and practical tips for switching from sulfonylureas to each of these alternatives. Whether you’re a patient looking for a safer pill or a prescriber fine‑tuning a regimen, the articles ahead will give you the facts you need to make an informed decision.

A side‑by‑side look at Glucovance versus Metformin alone, sulfonylureas, DPP‑4, SGLT2 and GLP‑1 drugs, covering efficacy, safety, cost and when to switch.
Lithium carbonate generics require careful serum level monitoring due to their narrow therapeutic index. Switching brands can alter blood levels, risking toxicity or relapse. Learn how formulation differences, dosing timing, and kidney function affect safety and effectiveness.

Navigating premature ejaculation in 2025 offers more options than ever before. This article explores eight alternatives to Priligy, highlighting the pros and cons of each. From psychotherapy to natural remedies, find out what might work best for you. Our insights include practical tips and interesting facts, aiming to support your journey toward better sexual health.

Learn how clinician portals and apps help healthcare providers detect adverse drug reactions in real time. Discover which tools work best for hospitals, clinical trials, and low-resource settings-and how to use them without burnout.

What androstenedione does, what studies show, real risks, and 2025 legal status. Clear, science-based guide with safer alternatives and a quick checklist.
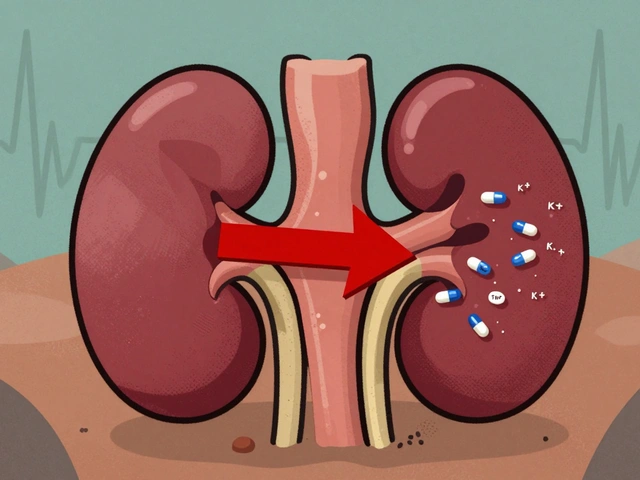
Trimethoprim can cause dangerous spikes in potassium levels, especially in older adults or those on blood pressure meds. Learn who's at risk, how to prevent life-threatening hyperkalemia, and safer antibiotic alternatives.