When you hear low salt diet, a dietary approach that limits sodium intake to support heart and kidney health. Also known as reduced sodium diet, it’s not just a trend—it’s a medically backed strategy used for people with high blood pressure, heart failure, or kidney disease. Most people eat way more sodium than they need—often over 3,400 mg a day—while health guidelines recommend under 2,300 mg, and sometimes as low as 1,500 mg for those with specific conditions.
The sodium intake, the amount of salt consumed daily, often from processed foods and restaurant meals directly affects how your body holds water. Too much sodium means your kidneys struggle to flush out excess fluid, which increases pressure in your blood vessels. That’s why doctors often recommend a low salt diet, a dietary approach that limits sodium intake to support heart and kidney health for people with hypertension, chronically elevated blood pressure that increases risk of stroke and heart attack. But it’s not just about blood pressure. People with hyponatremia, a condition where blood sodium levels drop too low, often due to excess fluid or certain medications need careful sodium management too—sometimes even adding salt back in, under medical supervision.
What’s surprising is how many meds tie into this. Drugs like Natrise (tolvaptan) are used to fix low sodium, but they only work if your diet isn’t sabotaging them. Same goes for diuretics—those water pills—your body’s response depends heavily on how much salt you’re eating. Even osteoporosis meds like bisphosphonates can be less effective if your sodium intake is too high, because excess salt pulls calcium out of your bones. It’s not just about skipping the chips. It’s about understanding how your food choices interact with your meds, your kidneys, and your heart.
Some think cutting salt means eating bland food, but that’s not true. Real change comes from swapping processed snacks for whole foods, reading labels on canned soups and sauces, and cooking at home more often. It’s not about perfection—it’s about progress. And when you combine a low salt diet with the right medication plan, the results can be real: lower blood pressure, less swelling, fewer hospital visits.
Below, you’ll find detailed comparisons of medications like Natrise and others that are used alongside dietary changes, plus guides on how sodium affects everything from bone health to hormone balance. Whether you’re managing high blood pressure, kidney issues, or just trying to eat smarter, these posts give you the facts—not the fluff.

Learn how to manage salt intake while taking ramipril to lower blood pressure, reduce side effects, and protect your heart and kidneys. Practical diet tips, hidden sodium sources, and what to avoid.

A practical guide comparing Duricef (cefadroxil) with common oral antibiotics, covering effectiveness, dosing, side‑effects, costs, and when to choose each option.
A comprehensive side‑by‑side comparison of female Viagra (sildenafil) with Addyi, Vyleesi, generic options and herbal alternatives, covering how they work, dosing, safety and when each is best.
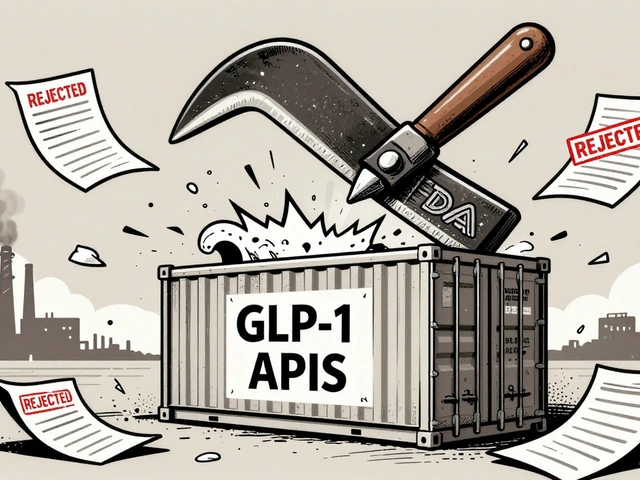
The FDA uses Import Alerts to automatically block drug shipments from non-compliant manufacturers. With the 2025 Green List initiative, enforcement against GLP-1 APIs has become the strictest in history-reshaping global supply chains and raising compliance standards.
Check your medicine cabinet twice a year to remove expired drugs and prevent accidents. Learn what to toss, where to store meds safely, and how to dispose of them the right way.
Explore why genotype 3 hepatitis C often causes stubborn fatigue, the biological reasons behind it, and practical steps to manage and recover from this symptom.