When you're taking ramipril, what you eat matters just as much as the pill you swallow. Ramipril is a common medicine for high blood pressure and heart failure, but it doesn’t work the way it should if your diet is full of salt. Too much sodium doesn’t just raise your blood pressure-it can make ramipril less effective, increase swelling, and even lead to dangerous spikes in potassium levels. This isn’t about cutting out salt completely. It’s about understanding how much you really need, where it hides, and how to eat smarter without feeling deprived.
Why Salt Matters with Ramipril
Ramipril belongs to a class of drugs called ACE inhibitors. These medicines help relax blood vessels and reduce fluid buildup in your body. But they also affect how your kidneys handle sodium and potassium. When you eat a lot of salt, your body holds onto water. That extra fluid pushes against your artery walls, raising your blood pressure. Ramipril tries to counteract that, but if you’re eating 3,000 mg of sodium a day, the medicine is fighting an uphill battle.
Studies show that people on ACE inhibitors like ramipril who reduce sodium intake see significantly better blood pressure control than those who don’t. One 2023 analysis of over 12,000 patients found that cutting sodium to under 2,000 mg per day improved systolic blood pressure by an average of 8 mmHg-similar to adding a second blood pressure pill. That’s not a small gain. It means fewer headaches, less strain on your heart, and lower risk of stroke or kidney damage.
There’s another hidden risk: high potassium. Ramipril can cause potassium to build up in your blood. Salt substitutes often contain potassium chloride instead of sodium chloride. If you’re using those to cut salt, you might be trading one problem for another. High potassium can cause irregular heartbeats, muscle weakness, or even cardiac arrest in severe cases.
How Much Salt Is Too Much?
The American Heart Association recommends no more than 2,300 mg of sodium per day for most adults-and ideally, no more than 1,500 mg if you have high blood pressure, heart failure, or kidney disease. That’s about two-thirds of a teaspoon of table salt. But most people eat way more than that. The average American consumes around 3,400 mg daily.
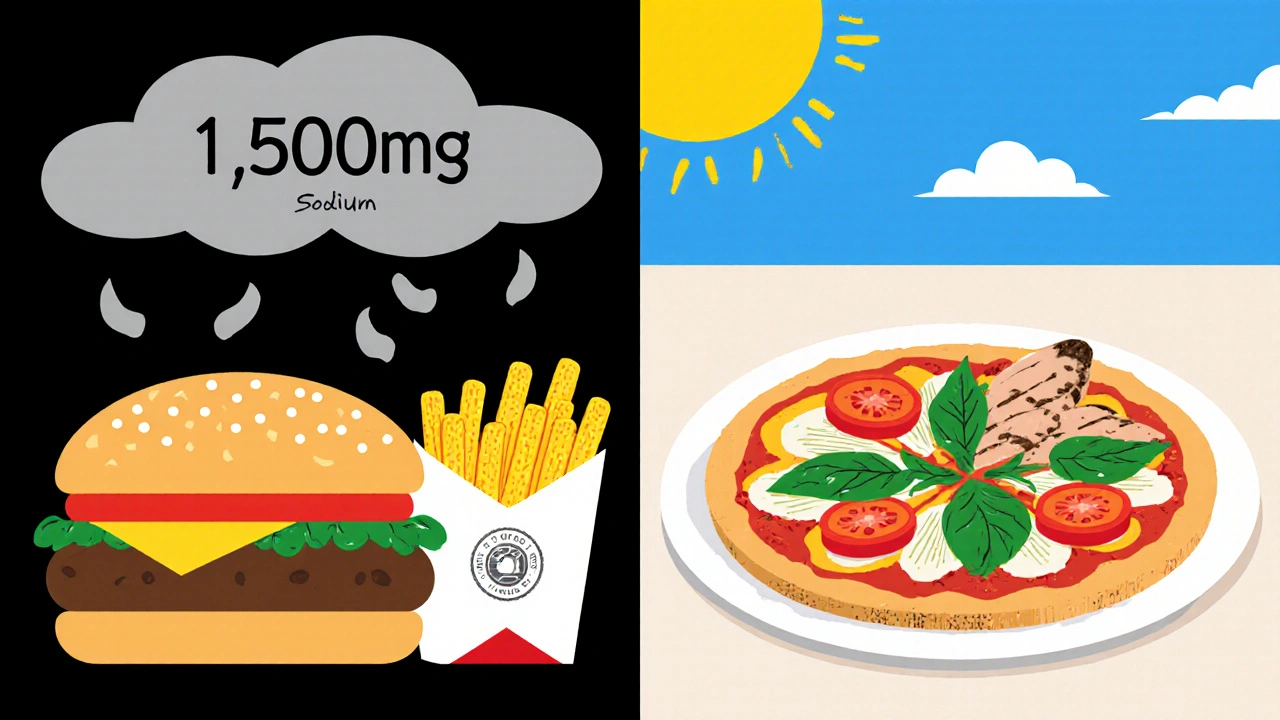
Here’s the catch: over 70% of that sodium doesn’t come from your salt shaker. It comes from packaged and restaurant food. A single slice of store-bought bread can have 230 mg. A cup of canned soup? 800 mg or more. A fast-food burger with cheese and sauce? Easily 1,500 mg before you even add fries.
So if you’re on ramipril, counting salt isn’t about avoiding the salt shaker. It’s about reading labels, choosing fresh foods, and learning what’s really in your meals.
What to Eat: A Simple Guide
You don’t need to become a nutritionist to eat well on ramipril. Start with these practical swaps:
- Choose fresh over processed. Fresh chicken, fish, vegetables, fruits, and whole grains have almost no sodium. Frozen vegetables without sauce are fine too. Avoid anything labeled “seasoned,” “marinated,” or “ready to heat.”
- Read nutrition labels. Look for “sodium” on the label. Aim for foods with less than 140 mg per serving. If a product has more than 300 mg per serving, think twice.
- Use herbs and spices instead of salt. Garlic, rosemary, cumin, paprika, lemon juice, and vinegar add flavor without sodium. Try a blend like Mrs. Dash or make your own with dried herbs.
- Don’t rinse canned foods. Rinsing beans or tuna reduces sodium by about 30-40%. It’s not perfect, but it helps.
- Watch out for hidden sodium. Soy sauce, ketchup, salad dressings, deli meats, and even some breakfast cereals are loaded. Look for “low sodium,” “no salt added,” or “unsalted” versions.
For example, instead of grabbing a frozen pizza (1,800 mg sodium), make a simple tomato and basil pizza with whole-wheat crust, fresh mozzarella, and no added salt. Top it with spinach and mushrooms. You’ll get flavor, fiber, and under 500 mg of sodium.
What to Avoid Completely
Some foods are just too risky when you’re on ramipril. Here’s what to skip or limit:
- Salt substitutes with potassium chloride. If you have kidney disease or take other medications that raise potassium (like spironolactone), these can be dangerous. Always check with your doctor before using them.
- Canned soups and broths. Even “low sodium” versions can have 400-600 mg per cup. Better to make your own broth with herbs and vegetables.
- Pickled and cured meats. Bacon, ham, salami, and hot dogs are packed with sodium and nitrates. Replace them with grilled chicken, turkey breast, or tofu.
- Fast food and takeout. A single meal from a chain restaurant can hit your entire daily sodium limit. If you must eat out, ask for sauces on the side, skip the cheese, and choose grilled options.
- Pre-packaged meals. Things like microwave dinners, instant noodles, and frozen lasagna are sodium bombs. Even “healthy” frozen meals often have over 1,000 mg per serving.
Tracking Your Progress
How do you know if you’re doing it right? Start by writing down what you eat for a week. Use a free app like MyFitnessPal or just a notebook. Look at your sodium totals. If you’re consistently over 2,000 mg, you’ve got work to do.
Also, pay attention to your body. Are your ankles swelling more than usual? Do you feel bloated after meals? Are you still getting headaches? These could be signs your sodium intake is still too high. Keep a log of symptoms along with your meals. Share it with your doctor at your next visit.
Some people see results in as little as two weeks. Blood pressure drops, energy improves, and swelling goes down. Others take longer. That’s normal. The goal isn’t perfection-it’s progress.
What About Potassium?
Ramipril can raise potassium levels, especially if you have kidney problems. That’s why you need to be careful with foods high in potassium-like bananas, oranges, potatoes, spinach, and tomatoes. But you don’t need to avoid them entirely.
The key is balance. If your kidneys are working fine and your doctor hasn’t warned you about potassium, you can still eat these foods in normal portions. One banana a day is fine. Two cups of spinach in a salad? Also fine. But don’t start drinking potassium supplements or eating huge amounts of dried fruit.
Your doctor should check your potassium levels with a simple blood test every few months, especially when you first start ramipril or if your dose changes. If your potassium is high, they’ll adjust your diet or meds accordingly.
Common Mistakes and How to Fix Them
Here are the top three mistakes people make when trying to cut salt on ramipril:
- Thinking “no salt” means no flavor. You can still eat delicious food. Use citrus, garlic, smoked paprika, and herbs. Try a splash of balsamic vinegar on roasted veggies. Flavor doesn’t need salt.
- Assuming “healthy” means low sodium. Granola bars, protein shakes, and whole-grain breads often have hidden salt. Always check the label.
- Giving up after a week. Taste buds adapt. After 4-6 weeks of eating less salt, you’ll start to notice how salty processed food really is. You’ll actually prefer the natural taste of food.
Don’t try to change everything overnight. Pick one thing to focus on each week. Week one: stop adding salt at the table. Week two: swap one processed snack for fresh fruit. Week three: cook one meal from scratch. Small steps add up.
When to Talk to Your Doctor
You should call your doctor if:
- Your blood pressure stays high despite taking ramipril and cutting salt.
- You feel dizzy, weak, or have an irregular heartbeat.
- Your legs or feet swell suddenly.
- You’re having trouble keeping up with your diet and need help.
Your doctor might adjust your ramipril dose, add another medication, or refer you to a dietitian. There’s no shame in asking for help. Managing blood pressure is a team effort-and your diet is a big part of that team.
Final Thoughts
Ramipril is a powerful tool for protecting your heart and kidneys. But it’s not magic. It works best when you give it a fighting chance-and that means eating food that doesn’t fight back. You don’t need to be perfect. You just need to be consistent. Cut back on salt, choose real food, read labels, and listen to your body. Over time, you’ll feel the difference-not just in your numbers, but in how you live every day.
Can I still eat out if I’m on ramipril?
Yes, but you need to be smart. Ask for sauces and dressings on the side, skip the cheese and bacon, choose grilled over fried, and avoid soups, stews, and anything labeled “seasoned.” Many restaurants now list sodium content online-check before you go. A simple grilled chicken salad with olive oil and vinegar is usually a safe bet.
Is sea salt better than table salt for ramipril?
No. Sea salt, kosher salt, and Himalayan salt all contain the same amount of sodium as table salt-about 40% sodium by weight. The texture and flavor might be different, but your body processes them the same way. Switching salt types won’t lower your sodium intake.
How long does it take for a low-salt diet to lower blood pressure?
Most people see a drop in blood pressure within 1 to 4 weeks of cutting salt. The bigger the change in sodium intake, the faster the result. Some see a 5-10 mmHg drop in systolic pressure in just two weeks. Consistency matters more than speed.
Can I drink alcohol while taking ramipril?
Moderate alcohol is usually okay-one drink a day for women, two for men-but it can lower blood pressure too much, especially when combined with ramipril. It can also make you dehydrated and increase dizziness. If you drink, do so slowly and monitor how you feel. Talk to your doctor if you’re unsure.
Should I take potassium supplements with ramipril?
No, unless your doctor specifically tells you to. Ramipril can raise potassium levels naturally. Taking extra potassium-through supplements or salt substitutes-can lead to dangerous levels. Always get your potassium checked with a blood test before considering any supplements.



Rebecca Parkos
November 3, 2025 AT 16:39I used to eat ramipril and salt like they were best friends-until my ankles swelled up like balloons. One day I just said ‘enough’ and started reading labels. Turned out my ‘healthy’ granola bar had more sodium than a bag of chips. I switched to fresh veggies, herbs, and lemon. Two weeks later, my BP dropped 12 points. No joke. You don’t need to be perfect, just consistent. And yeah, I still eat out-I just ask for no salt, no sauce, and side-eye the waiter if they try to sneak it in.
Bradley Mulliner
November 4, 2025 AT 21:21Let’s be real-most people who complain about salt are just too lazy to cook. If you can’t handle reading a nutrition label, maybe you shouldn’t be on blood pressure medication. And don’t even get me started on those ‘low sodium’ packaged foods-they’re just marketing lies wrapped in plastic. The real issue? People think medicine fixes everything. It doesn’t. You fix your life-or you die early. Simple as that.
Rahul hossain
November 5, 2025 AT 09:32Respected author, your article is a beacon in the fog of misinformation. In India, we have long understood the wisdom of ‘namak kam, zindagi zyada’-less salt, more life. Yet modern diets, driven by corporate convenience, have eroded this. I have seen elderly patients on ACE inhibitors, consuming pickles daily, then blaming the drug for their stroke. The solution is not pharmaceutical-it is cultural. Teach children to taste food, not drown it. A pinch of black pepper, a dash of turmeric, the scent of cumin in hot oil-this is flavor, not poison. Let us reclaim the kitchen.
Reginald Maarten
November 6, 2025 AT 16:59Actually, the 2,300 mg sodium recommendation is outdated. The 2023 meta-analysis you cited? It included patients with comorbidities-most of whom were sedentary, diabetic, or obese. The effect size was negligible in healthy, active individuals. Also, potassium chloride substitutes aren’t inherently dangerous-they’re dangerous if you have renal impairment. But you didn’t mention glomerular filtration rate (GFR), which is the actual clinical determinant. And ‘rinsing canned beans reduces sodium by 30–40%’? That’s misleading. It’s 25–35% depending on the bean type and rinse duration. Precision matters.
Jonathan Debo
November 8, 2025 AT 00:16Let’s be crystal-clear: Sea salt is not ‘better’-it’s identical in sodium content. And ‘low-sodium’ broth? Often contains yeast extract, which is just hidden MSG. You’re not fooling anyone. Also, ‘use herbs and spices’? That’s the most patronizing advice ever. Do you know how expensive saffron is? Or how many people live in food deserts? This article reads like a Whole Foods ad written by someone who’s never cooked a meal in their life. And why no mention of diuretics? You’re treating symptoms, not systems.
Robin Annison
November 9, 2025 AT 22:00I’ve been on ramipril for five years. What changed me wasn’t the science-it was the silence. I used to eat like I was racing against time: frozen dinners, canned soup, chips between meetings. One night, I sat down with a bowl of lentils, garlic, and cumin, and just… listened. To the steam. To the quiet. To my body not feeling like a balloon. I didn’t lose weight. I didn’t become a chef. But I started to feel like I was alive, not just surviving. That’s the real win. Not the numbers. The feeling.
Abigail Jubb
November 10, 2025 AT 23:12I cried reading this. Not because I’m dramatic-though I am-but because I realized I’ve been poisoning myself for 12 years. My mom died of heart failure at 58. I thought it was ‘just genetics.’ Turns out, it was the deli meat. The frozen pizza. The soy sauce. I just… didn’t know. I’ve thrown out every spice blend with salt since yesterday. I’m making my own broth. I’m terrified. But I’m also… hopeful. For the first time in a decade, I feel like I have control.
George Clark-Roden
November 12, 2025 AT 07:56There’s a quiet revolution happening here-not in labs or hospitals, but in kitchens. When you stop seeing food as fuel or punishment, and start seeing it as conversation-with your body, with your ancestors, with your future self-you change. Ramipril isn’t a magic bullet. It’s a bridge. And the bridge is made of tomatoes you roasted yourself, of beans you rinsed with care, of garlic you crushed with your fingers. The salt shaker? It’s not the enemy. It’s the ghost of a habit you outgrew. And that’s beautiful.
Hope NewYork
November 14, 2025 AT 07:52Bonnie Sanders Bartlett
November 16, 2025 AT 04:08I’m a nurse, and I’ve watched people turn their lives around with small changes. One woman swapped her canned soup for homemade veggie stew. Another stopped putting salt on her eggs. They didn’t become chefs. They didn’t buy fancy gadgets. They just chose one thing to do better. And over time? Their energy came back. Their shoes fit again. Their spouses noticed. You don’t need a plan. You just need to start. One meal. One label. One day. That’s all it takes.
Melissa Delong
November 17, 2025 AT 05:22Who funds this article? Big Pharma? The salt industry? Did you know that the American Heart Association gets donations from food conglomerates? The real reason ramipril works better with low sodium? Because if you don’t control diet, you need more drugs. And more drugs = more profit. I’ve seen patients get switched to potassium-sparing diuretics-then their potassium spiked. Was it the diet? Or the combo of meds? Nobody asks. They just blame the patient. Wake up.
Marshall Washick
November 17, 2025 AT 09:18I’ve been on ramipril since my heart attack. I used to think cutting salt meant eating cardboard. Then I tried smoked paprika and a squeeze of lime on grilled fish. It tasted like the ocean. I started cooking with my daughter-she’s 10. We make chili with black beans, no salt, just cumin and chocolate. She says it’s ‘spicy magic.’ I don’t care if it’s perfect. I care that we’re together, and I’m alive to see her grow. Ramipril didn’t save me. The quiet dinners did.