Medication-Induced Glaucoma Risk Assessment Tool
Assess Your Risk
This tool estimates your risk of medication-induced acute angle-closure glaucoma based on key risk factors identified in medical research. The more risk factors you have, the higher your risk.
Risk Factors
Your Risk Assessment
Imagine waking up with blinding eye pain, halos around lights, and nausea-then realizing your headache wasn’t a migraine, but your eye pressure had spiked to 60 mm Hg. That’s what happens in acute angle-closure glaucoma triggered by common medications. It’s not rare. It’s not theoretical. It’s a preventable emergency that blinds people every day because no one connected the dots between a cold pill and sudden vision loss.
What Exactly Is Medication-Induced Acute Angle-Closure Glaucoma?
Acute angle-closure glaucoma (AACG) happens when the drainage angle inside your eye-where fluid normally flows out-suddenly closes. This traps fluid inside, causing pressure to skyrocket. Normal eye pressure is 10-21 mm Hg. In this emergency, it can hit 40-80 mm Hg. Within hours, the optic nerve starts dying. Permanent vision loss can happen in under 24 hours.
What makes this different from the more common open-angle glaucoma? Open-angle glaucoma creeps up silently over years. Medication-induced AACG hits like a sledgehammer. It doesn’t wait. It strikes fast, often in people who never knew they were at risk.
The trigger? Medications. Not all meds. But specific ones. And they don’t need to be eye drops. A nasal spray, an allergy pill, or an antidepressant can be enough. The problem isn’t the drug itself-it’s what it does to your eye anatomy.
Who’s at Risk? It’s Not Just Older Adults
You don’t have to be over 60. You don’t have to have a family history of glaucoma. The real risk factor is your eye shape.
People with shallow anterior chambers (less than 2.5 mm deep), narrow iridocorneal angles, or who are farsighted are sitting ducks. Asian populations have a higher risk-8.5% have narrow angles compared to 3.8% in White populations. That’s more than double.
And here’s the scary part: only about 25% of people who develop medication-induced AACG even know they have narrow angles. Most never had a screening. No one told them. They took a medication they’d used before-no problem. Until it wasn’t.
The Top 5 Culprit Medication Classes
Not all drugs are dangerous. But these five classes are known to trigger AACG:
- Adrenergic agents - Especially phenylephrine (10% eye drops or nasal sprays). This is the #1 offender, causing 35% of cases. Found in decongestants, eye redness relievers, and even some cold medicines.
- Anticholinergics - Tropicamide (used in eye exams), diphenhydramine (Benadryl), and scopolamine. These cause pupil dilation, which physically blocks the drainage angle. Tropicamide alone is responsible for 28% of cases.
- Sulfonamide-based drugs - Acetazolamide, sulfamethoxazole, topiramate. These can cause swelling in the ciliary body, pushing the iris forward and closing the angle. The FDA now requires black box warnings on topiramate and sulfa drugs for this reason.
- Serotonergic antidepressants - SSRIs like paroxetine and fluoxetine. Though less common, they account for 12% of cases. The mechanism isn’t fully understood, but it’s linked to pupil changes and ciliary body effects.
- Antihistamines and decongestants - Pseudoephedrine, phenylephrine in oral form. These are OTC staples. People take them daily for allergies or colds-and don’t realize they’re playing Russian roulette with their vision.
Some drugs, like anticholinergics, attack in two ways: they dilate the pupil AND cause iris swelling. That’s a double hit. Sulfa drugs don’t just dilate-they swell the ciliary body, physically pushing the iris forward. It’s not one mechanism. It’s a cascade.
What Does an Attack Feel Like?
If you’re in the middle of one, you won’t think it’s ‘just a headache.’ Symptoms come on fast-within minutes to hours after taking the drug:
- Severe eye pain, often radiating to the forehead or temple
- Blurred or cloudy vision
- Seeing rainbow-colored halos around lights
- Red, swollen eye
- Nausea and vomiting
- Fixed, mid-dilated pupil (4-6 mm) that doesn’t react to light
Many patients go to the ER thinking it’s a migraine or sinus infection. A 2021 JAMA Ophthalmology study found that non-eye doctors correctly diagnose AACG in only 38% of cases. The average delay in diagnosis? 17 hours. That’s 17 hours where pressure is crushing the optic nerve.
One patient on the Glaucoma Research Foundation forum said: “I took pseudoephedrine for allergies. Three hours later, I couldn’t see clearly. The ER gave me painkillers. I lost 20% of my peripheral vision before an ophthalmologist figured it out.”
How Is It Treated? Time Is Everything
There’s no waiting. No “let’s monitor it.” This is a 911 situation.
Immediate treatment starts with lowering eye pressure:
- Pilocarpine 2% - Drops every 15 minutes for an hour. This shrinks the pupil, pulling the iris away from the drainage angle.
- Intravenous mannitol - A powerful osmotic agent that pulls fluid out of the eye. Used in hospitals when pressure is above 50 mm Hg.
- Carbonic anhydrase inhibitors - Oral or IV acetazolamide to reduce fluid production.
Once pressure is under control, the definitive fix is a laser peripheral iridotomy. A tiny hole is burned in the iris to let fluid flow freely again. This is done within 24 hours to prevent recurrence.
But here’s the truth: even with perfect treatment, some people lose vision permanently. The damage isn’t reversible. That’s why prevention is the only real win.
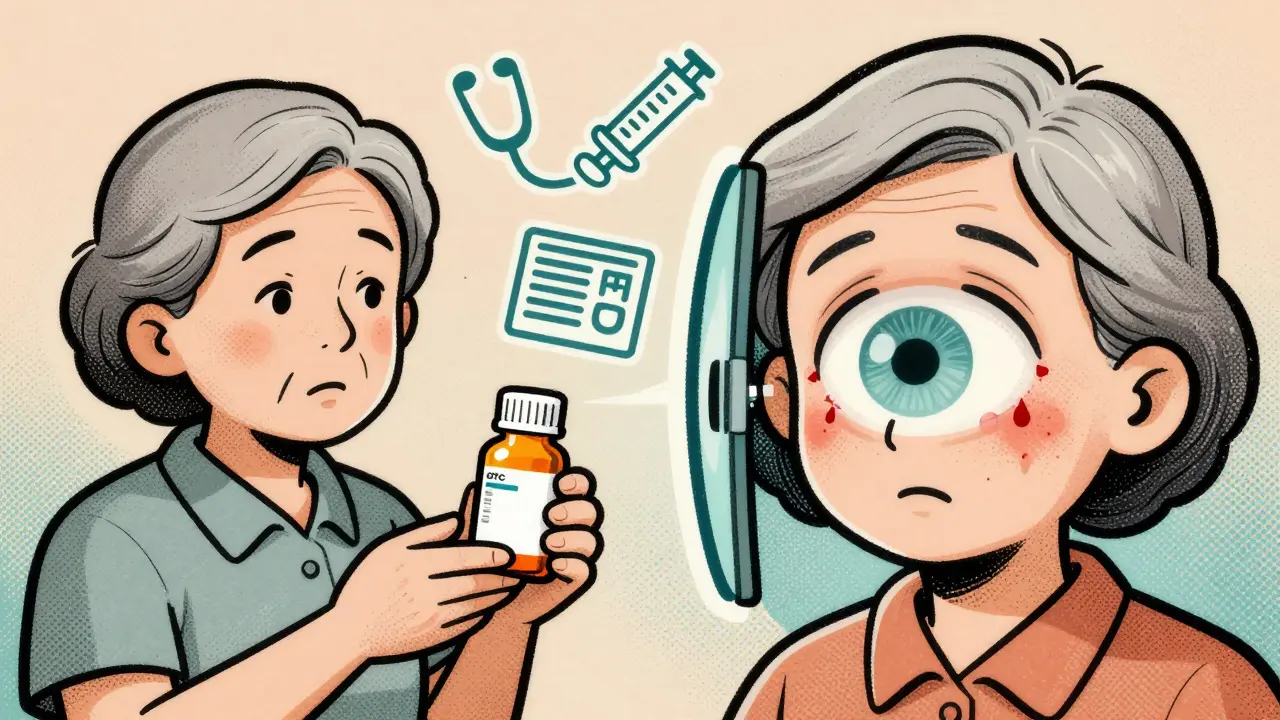
How to Prevent It Before It Happens
This isn’t a mystery. We know who’s at risk. We know which drugs trigger it. We have tools to screen for it.
The American Academy of Ophthalmology recommends a simple 5-7 minute test called gonioscopy for anyone over 40 before prescribing high-risk meds. It uses a special lens to directly see the drainage angle. If the angle is narrow (Shaffer grade ≤2), you avoid the dangerous drugs.
There are safe alternatives:
- Instead of diphenhydramine (Benadryl), use loratadine (Claritin) or cetirizine (Zyrtec).
- Instead of pseudoephedrine, use phenylephrine-free cold meds or saline nasal sprays.
- For asthma, use formoterol instead of epinephrine.
- For depression, consider non-serotonergic options like bupropion if you have narrow angles.
Electronic health records now have alerts. Epic Systems added glaucoma risk flags in 2022. But only 42% of primary care doctors routinely screen. And 68% of patients say they were never warned about eye risks when prescribed these meds.

Why This Keeps Happening
We have the knowledge. We have the tools. So why are people still losing vision?
Because the system doesn’t connect the dots. Primary care doctors prescribe the meds. Optometrists see the eyes. Pharmacists fill the prescriptions. No one talks. No one checks.
Patients aren’t told. They assume “if my doctor prescribed it, it’s safe.” They don’t know that a routine eye exam with dilating drops can trigger an attack if their angles are narrow.
One Reddit user wrote: “My eye doctor used tropicamide without checking my angle width first. I woke up with 60 mm Hg pressure. Permanent damage.”
This isn’t malpractice in the criminal sense. It’s systemic neglect. A gap in communication. A lack of standardized screening. A failure to treat eye anatomy as seriously as blood pressure or cholesterol.
What You Can Do Right Now
If you’re over 40, or if you’re farsighted, or if you’re of East Asian descent-ask your eye doctor: “Have my drainage angles been checked?”
If you’re prescribed any of the high-risk medications listed above-ask: “Could this affect my eyes?”
If you’ve ever had sudden eye pain, blurred vision, or halos after taking a new medication-seek an ophthalmologist immediately. Don’t wait. Don’t assume it’s a migraine.
And if you’re a caregiver for someone older or with chronic conditions-know these drugs. Keep a list. Ask questions. Advocate.
This isn’t about fear. It’s about awareness. You can’t prevent what you don’t understand. But now you do.
What’s Next? The Future of Prevention
Optical coherence tomography (OCT) can now map the drainage angle with 94% accuracy-faster and easier than gonioscopy. Genetic testing is emerging too. The GLAUGEN Consortium found 17 genetic markers linked to narrow angles. In 10 years, a simple blood test might tell you your risk.
But for now, the tools we have are free, fast, and proven. Gonioscopy. Patient education. Medication alternatives. Communication between providers.
The question isn’t whether we can stop this. It’s whether we will.