When you or your child gets sick with a fever, sore throat, or cough, the biggest question isn’t just how bad it is-it’s what’s causing it. Is it bacteria? Or a virus? The answer changes everything: what you take, how long you’re sick, and even whether you risk contributing to a global health crisis.
Here’s the hard truth: most people can’t tell the difference. A 2023 CDC survey found that 68% of adults think antibiotics can cure the flu. They can’t. And that misunderstanding is making superbugs stronger every year.
What’s the Real Difference Between Bacteria and Viruses?
Bacteria are alive. They’re single-celled organisms that can eat, grow, and multiply on their own-even on a doorknob or in soil. They reproduce by splitting in half, sometimes every 20 minutes under the right conditions. That’s why a strep throat infection can go from mild to severe in just a day or two.
Viruses aren’t alive in the traditional sense. They’re just genetic material wrapped in a protein shell. They can’t do anything on their own. They need to sneak into your cells and hijack their machinery to copy themselves. That’s why you can’t catch a cold from a contaminated surface alone-you need to breathe in the virus, or touch your face after it’s on your hand.
Size matters too. The biggest viruses are about 300 nanometers wide. The smallest bacteria are around 200 nanometers. That’s why you can’t see bacteria with a regular microscope-but you still can’t see viruses without an electron microscope. That’s why doctors can’t just look at a throat and know if it’s bacterial or viral.
Common Infections: What’s Bacterial? What’s Viral?
Not all infections are created equal. Some are almost always one or the other.
Bacterial infections:
- Strep throat (caused by Group A Streptococcus)-affects over 600 million people worldwide each year
- Tuberculosis-10.6 million new cases in 2022, mostly in low-income countries
- Urinary tract infections (UTIs)-8.1 million doctor visits in the U.S. annually
- Sinus infections (when they’re bacterial)-about 30% of cases
- Whooping cough (pertussis)-still common in unvaccinated populations
Viral infections:
- Common cold (rhinoviruses)-most people get 2-4 per year
- Influenza (flu)-9 to 41 million cases in the U.S. every year
- COVID-19-over 7 million documented deaths globally as of May 2024
- Chickenpox (varicella-zoster)-4 million cases yearly before vaccines
- Mononucleosis (Epstein-Barr virus)-often mistaken for strep in teens
Here’s the tricky part: you can get a viral cold, then develop a bacterial sinus infection on top of it. That’s why symptoms that get better, then suddenly get worse, are a red flag.
How Symptoms Differ (And Why They Don’t Always Help)
Doctors don’t rely on symptoms alone. But knowing what to watch for helps you ask better questions.
More likely bacterial:
- Fever above 101°F (38.3°C)
- Symptoms lasting more than 10-14 days
- Worsening after initial improvement (like a cold turning into a sinus infection)
- Pus on tonsils or thick, colored mucus that lasts more than a week
More likely viral:
- Fever under 100.4°F (38°C)
- Runny nose, sneezing, mild cough
- Body aches and fatigue
- Improvement within 7-10 days
But here’s the catch: flu (viral) can spike your fever to 103°F. And some bacterial infections, like early Lyme disease, start with mild fever and fatigue. That’s why testing matters.
Testing: How Doctors Actually Know the Difference
There’s no magic trick. But there are reliable tests.
For strep throat, a rapid antigen test gives results in 10 minutes with 95% accuracy. If it’s negative but the doctor still suspects strep, they’ll send a throat culture-which takes 24-48 hours but is 98% accurate.
For flu, a PCR test done within the first 72 hours of symptoms is 90-95% accurate. For COVID-19, rapid antigen tests are good for detecting active infection, especially if you have symptoms.
And now there’s a new tool: FebriDx. Approved by the FDA in 2020, it’s a finger-prick blood test that checks two markers-CRP (inflammation) and MxA (a protein made only during viral infections). It’s 94% sensitive and 92% specific. In primary care clinics, it’s cut unnecessary antibiotic prescriptions by half.
But these tests aren’t perfect. They’re not always available, and they cost money. That’s why doctors use tools like the Centor Criteria to estimate risk before testing:
- Tonsil exudate (white patches) = 1 point
- Tender neck lymph nodes = 1 point
- Fever over 100.4°F = 1 point
- No cough = 1 point
If you score 3 or higher, there’s a 50-55% chance it’s strep. That’s when testing makes sense.
Treatment: Antibiotics vs. Antivirals vs. Rest
This is where most people get it wrong.
Bacterial infections need antibiotics. But not just any antibiotic. Strep throat? Penicillin or amoxicillin for 10 days. UTI? Nitrofurantoin or trimethoprim-sulfamethoxazole. Tuberculosis? A combo of 3-4 drugs for 6-9 months.
Why 10 days for strep? Because stopping early lets the toughest bacteria survive-and they come back stronger. That’s how antibiotic resistance starts.
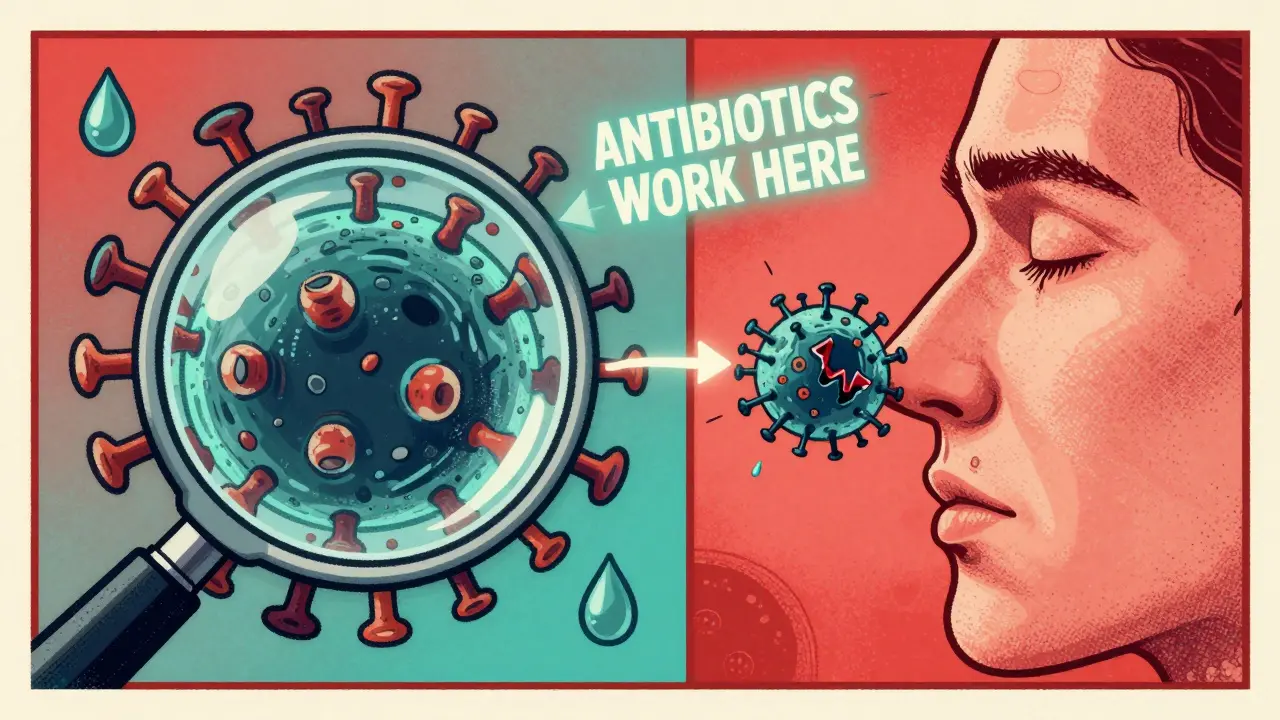
Viral infections don’t respond to antibiotics. Period. That’s not opinion-it’s biology. Viruses don’t have cell walls. They don’t make proteins the same way. Antibiotics target bacterial machinery. They’re useless against viruses.
So what do you do?
- Rest
- Hydrate
- Use acetaminophen or ibuprofen for fever and pain
There are exceptions. Oseltamivir (Tamiflu) for flu can shorten illness by 1-2 days-if taken within 48 hours of symptoms. Remdesivir helps hospitalized COVID-19 patients. Acyclovir reduces severity of chickenpox and shingles.
But for 90% of viral infections? There’s no pill. Just time.
Why Taking Antibiotics for a Virus Is Dangerous
Every time you take an antibiotic when you don’t need it, you’re helping bacteria evolve.
Antibiotic resistance isn’t science fiction. It’s happening now. In 2019, drug-resistant infections killed 1.27 million people worldwide. By 2050, that number could hit 10 million-more than cancer.
In the U.S., 47 million unnecessary antibiotic prescriptions are written every year. Most are for viral colds, coughs, and sore throats.
And the side effects? Diarrhea. Allergic reactions. And Clostridioides difficile (C. diff), a deadly gut infection caused when antibiotics wipe out good bacteria. In 2022, C. diff caused over 223,000 infections and 12,800 deaths in the U.S. alone.
It gets worse. People who get unnecessary antibiotics are 65% more likely to return to the doctor for the same symptoms next time. Why? Because they expect a pill. And when they don’t get one, they assume the doctor missed something.
What You Can Do Right Now
Don’t pressure your doctor for antibiotics. Don’t demand them because you’re tired of being sick. Don’t take leftover antibiotics from last winter’s cold.
Ask these questions instead:
- Is this likely bacterial or viral?
- Do we need a test to be sure?
- What can I do to feel better without antibiotics?
- When should I come back if it doesn’t improve?
And if you’re a parent: kids get 6-8 viral respiratory infections a year. That’s normal. It doesn’t mean their immune system is weak. It means they’re building it.
One study found that 85% of bronchitis cases and 70% of sinus infections in kids are viral. Antibiotics won’t help. And they might hurt.
The Bigger Picture: What’s Changing in Infection Care
Science is catching up. Researchers at the University of Queensland are testing two new compounds, IMB-001 and IMB-002, that target bacterial surface proteins-potentially bypassing resistance mechanisms. They’re in Phase II trials as of late 2024.
Phage therapy-using viruses that kill bacteria-is showing 85% success in European trials for resistant infections. It’s not mainstream yet, but it’s coming.
And vaccines? They’re the ultimate weapon. Flu shots, pneumococcal vaccines, and now universal coronavirus vaccines in Phase III trials could prevent entire waves of illness before they start.
The WHO says antibiotic resistance is one of the top 10 global health threats. The UN warns we’re on track for 10 million deaths a year from superbugs by 2050.
But here’s the good news: you don’t need a lab coat to help. Just understand the difference between bacteria and viruses. And refuse antibiotics when they won’t help.

Haley Graves
January 16, 2026 AT 00:06Stop asking for antibiotics like they’re candy. If your kid has a runny nose and a low-grade fever for five days, it’s not bacterial. It’s just life. Rest, fluids, and patience are the real medicine here. The overprescribing has to stop, and it starts with us.
Jaspreet Kaur Chana
January 16, 2026 AT 06:43I grew up in Punjab where grandmas would brew turmeric milk and say, 'Let the fever burn out the bad.' We didn’t have rapid strep tests back then, but we knew when to wait and when to rush to the clinic. Now I see Americans popping amoxicillin for sniffles like it’s a vitamin. It’s not just dangerous-it’s culturally blind. Antibiotics aren’t a quick fix, they’re a last resort. Our ancestors understood that. Maybe we need to remember.
ellen adamina
January 18, 2026 AT 04:48I had C. diff after a 3-day course of amoxicillin for a sore throat that turned out to be viral. I spent three weeks in bed. I lost 15 pounds. My gut hasn’t been the same since. No one warned me. No one even asked if I’d taken antibiotics before. This isn’t just about resistance-it’s about personal destruction.
Jami Reynolds
January 20, 2026 AT 00:25FebriDx? That’s a corporate placebo. The FDA approves these things because Big Pharma owns them. The real reason antibiotics are overprescribed? Doctors get paid more to write scripts than to explain biology. And the CDC? They’re funded by the same companies that sell antibiotics. This isn’t science-it’s a financial racket disguised as public health.
Iona Jane
January 21, 2026 AT 03:06They’re coming for our antibiotics and our freedom. First they take your Tylenol, then your ibuprofen, then they’ll tell you you’re not allowed to have a fever because it’s 'unhealthy.' The WHO wants to control every cough, every sneeze, every sniffle. They’re building a surveillance state under the guise of 'antibiotic stewardship.' Wake up. This is step one.
Nishant Garg
January 21, 2026 AT 07:12Back home in Delhi, we call it 'jwara'-fever. No one rushes to the doctor. We wait. We sip ginger tea. We let it run its course. If it doesn’t improve in 5 days? Then we go. No one’s handing out pills like confetti. We don’t panic. We adapt. Maybe the West needs to learn that less is more. Sometimes the body knows better than the prescription pad.
Nilesh Khedekar
January 21, 2026 AT 18:57Oh wow, so you’re saying I shouldn’t just take my brother’s leftover amoxicillin for my 'sinus thing'? What a shocker. Next you’ll tell me I shouldn’t Google symptoms and self-diagnose with WebMD. And that I shouldn’t expect a doctor to hand me a magic pill because I paid $200 for a 12-minute visit. How dare you question the sacred ritual of the antibiotic handshake!
Niki Van den Bossche
January 22, 2026 AT 00:13What’s truly fascinating is the epistemological collapse of medical literacy in the post-industrial West. We’ve outsourced our bodily autonomy to pharmacological intermediaries, mistaking pharmaceutical intervention for healing itself. The viral-bacterial dichotomy isn’t merely clinical-it’s ontological. We’ve forgotten that illness is not a technical malfunction to be rectified, but a dialogue between organism and environment. The antibiotic fetish is the symptom of a civilization that no longer trusts its own biology.
Jan Hess
January 22, 2026 AT 08:12Love this breakdown. Seriously. I used to beg for antibiotics every time I got a cough. Now I ask my doc: 'Is this viral? What can I do to feel better without pills?' They’re surprised-but they appreciate it. It’s not about being anti-medical. It’s about being smart with it. Small changes add up.
Diane Hendriks
January 22, 2026 AT 20:57It’s not just antibiotic misuse-it’s the erosion of linguistic precision. 'Infection' is not synonymous with 'sickness.' 'Viral' is not 'contagious.' 'Antibiotic' is not 'medicine.' The casual conflation of terms reflects a deeper societal decay in scientific literacy. If you can’t distinguish between a bacterium and a virus, you have no business making medical decisions. This is why the West is collapsing.
Gloria Montero Puertas
January 23, 2026 AT 23:39Of course you’re going to get a sinus infection after a cold-it’s not a coincidence, it’s a design flaw. The government allows viruses to spread so that we’ll flock to pharmacies and hospitals. They profit from your suffering. And now they want you to believe in 'FebriDx' like it’s some kind of miracle? Please. They’re just trying to make the scam look more scientific.
Tom Doan
January 25, 2026 AT 01:53Interesting how the article mentions phage therapy as 'coming soon'-but ignores that it’s been used successfully in Georgia since the 1920s. The West didn’t invent medicine. We just monopolized it. And now we’re surprised when our own arrogance creates superbugs? The irony is almost poetic.