Steroid Myopathy Strength Checker
Functional Strength Assessment
Test your muscle strength using the timed chair rise test recommended by clinical guidelines.
When you're on long-term steroids for asthma, rheumatoid arthritis, or another chronic condition, you might notice something strange: you can't stand up from a chair without using your hands. Climbing stairs feels impossible. Lifting your arms to reach a shelf becomes a struggle. And yet, there's no pain. No swelling. No red flags that scream "something's wrong." That’s the silent trap of steroid myopathy.
This isn't just feeling tired. It's a real, measurable loss of muscle strength caused by corticosteroids like prednisone, dexamethasone, or cortisone. It’s not rare - studies show 2.4% to 21% of people on chronic steroid therapy develop it. And because it happens slowly, doctors and patients often mistake it for just "getting older" or "the disease getting worse." But it’s not your illness. It’s the treatment.
How Steroids Attack Your Muscles
Steroids don’t just reduce inflammation. They also mess with how your muscles build and break down protein. At the cellular level, they turn on genes that trigger muscle breakdown - especially in fast-twitch muscle fibers, the ones you use to stand up, climb stairs, or lift things. At the same time, they shut down the signals that tell your muscles to grow. The result? Muscle wasting, without inflammation.
Unlike other muscle diseases, steroid myopathy doesn’t raise your creatine kinase (CK) levels. That’s a key clue. If your CK is normal - usually between 30 and 170 U/L - and you’re weak but not in pain, steroid myopathy is likely. EMG tests also look normal. No "early recruitment" patterns. No signs of inflammation. That’s why it’s so often missed.
Who’s at Risk?
If you’re taking more than 10 mg of prednisone daily for four weeks or longer, you’re in the risk zone. Higher doses - 40 to 60 mg - can cause problems in just two to three weeks, especially in ICU patients on IV steroids. People with COPD, asthma, lupus, or autoimmune diseases are most commonly affected. Dexamethasone is especially risky, particularly in kids with leukemia, because its chemical structure makes it more damaging to muscle tissue.
And here’s the kicker: even if you feel fine, your muscles might already be weakening. A 2019 study found that 78% of patients who tested normal on manual muscle exams had real strength deficits when measured with a dynamometer. That’s a machine that measures force precisely. Manual checks - like asking you to push against the doctor’s hand - often miss early changes.
How to Spot It Before It’s Too Late
There are simple, reliable tests you can ask your doctor or physical therapist to do:
- Timed Chair Rise Test: How long does it take you to stand up from a standard chair five times without using your arms? Normal is under 10 seconds. Over 15 seconds? That’s a red flag.
- Gower’s Maneuver: Can you get up from the floor without using your hands? If you have to push with your arms, roll onto your stomach, and slowly crawl up, that’s classic.
- Shoulder Abduction Test: Try lifting your arms out to the side. If you can’t get them past shoulder height without shrugging or bending your elbows, your deltoids are weakening.
These tests are 89% sensitive for catching steroid myopathy early. That means they catch almost all cases before they become severe. Yet, only 32% of rheumatology clinics and 27% of pulmonology practices use them routinely. Don’t wait for your doctor to notice - bring these up yourself.
What Patients Are Saying
On patient forums, the same stories keep coming up. One Reddit user wrote: "I had no pain, but I couldn’t get up from my couch without pushing off with my hands. Everyone thought I was just lazy. I felt like I was losing my body, piece by piece." Another from the Myositis Support Group said: "I used to play with my grandkids. Now I can’t pick them up. I cry every time I see them run past me." Sixty-eight percent of patients in a 2022 survey waited over five months to get the right diagnosis. That delay costs more than time - it costs mobility, independence, and confidence.
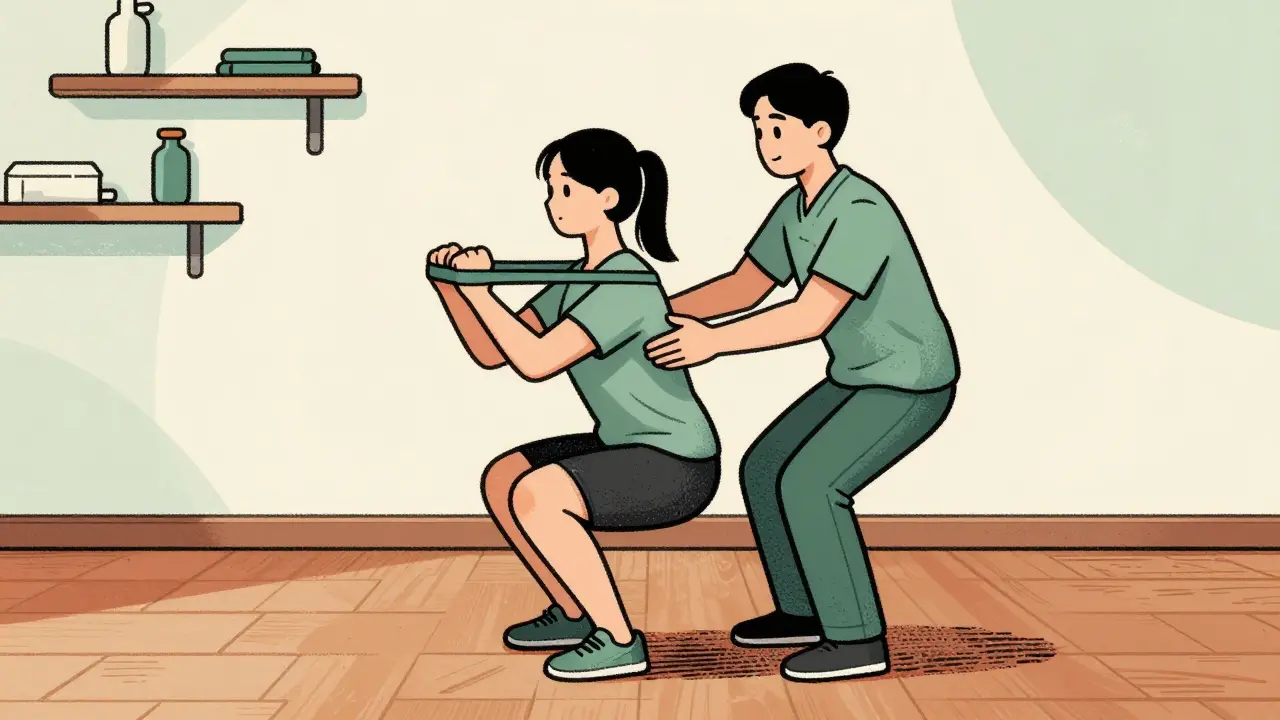
Physical Therapy That Actually Works
Here’s the good news: you can rebuild strength. But not with high-intensity workouts or heavy weights. That can make things worse.
Research shows that moderate, supervised resistance training is the most effective treatment. The American Physical Therapy Association recommends:
- 2-3 sessions per week
- 40-60% of your one-rep max (1RM)
- Focused on legs and hips first - quads, glutes, hamstrings
- Slow progression: increase weight by 5-10% every two weeks
A 2020 clinical trial gave 45 patients this exact plan for 12 weeks. Their chair rise time improved by 23.7%. The control group - who just did stretching - improved by only 8.2%. No injuries. No setbacks.
Start light. Even 30% of your 1RM is enough at first. Use resistance bands, bodyweight squats, seated leg presses, or wall sits. Avoid high-impact moves like jumping or sprinting. Your goal isn’t to push to failure - it’s to gently rebuild muscle protein without triggering breakdown.
What to Avoid
Some people think they need to "get stronger fast" and go all-out at the gym. That’s dangerous. High-intensity exercise increases muscle damage in steroid myopathy. Studies show it can accelerate protein breakdown, making weakness worse.
Also avoid prolonged bed rest. Inactivity makes muscle loss worse. Even walking 15-20 minutes a day helps maintain circulation and muscle tone. Don’t wait for your strength to come back before moving - move to make it come back.
What’s New in Treatment
There’s hope on the horizon. A new class of drugs called selective glucocorticoid receptor modulators (SEGRMs) is being tested. One, called Vamorolone, has shown 40% less muscle weakness than prednisone in clinical trials - while keeping the same anti-inflammatory power. It’s not widely available yet, but Phase III trials are underway.
The 2023 International Myopathy Guidelines Consortium is also finalizing the first-ever standardized physical therapy protocol for steroid myopathy. That means better training for therapists and clearer guidance for patients soon.
What You Can Do Today
Don’t wait for your next appointment. Take action now:
- Ask your doctor for a timed chair rise test or Gower’s maneuver.
- Request a referral to a physical therapist experienced in neuromuscular conditions.
- Start with two 20-minute sessions a week: bodyweight squats, step-ups, and seated leg extensions.
- Track your progress. Write down how many times you can stand from a chair without hands each week.
- Don’t stop your steroids unless your doctor says so - but do ask if your dose can be lowered safely.
Steroid myopathy isn’t your fault. It’s a side effect of a drug that saves lives. But it doesn’t have to steal your mobility. Recognizing it early and starting the right therapy can mean the difference between staying independent and needing help for everyday tasks.
The science is clear. The tools are available. You just need to ask the right questions - and start moving.
Can steroid myopathy be reversed?
Yes, in most cases. Muscle strength can improve significantly with consistent, moderate resistance training, even while continuing steroid therapy. Recovery takes time - usually 3 to 6 months - but studies show up to 25% improvement in functional strength within 12 weeks of starting physical therapy. Stopping steroids isn’t always necessary, and in many cases, reducing the dose slowly under medical supervision helps.
Is steroid myopathy painful?
No. That’s one of the key signs. Unlike inflammatory muscle diseases like polymyositis, steroid myopathy causes painless weakness. You won’t feel soreness, burning, or stiffness. The weakness comes on slowly, and you might not notice it until you can’t stand up from a chair without using your arms. This lack of pain is why it’s often mistaken for aging or deconditioning.
Do I need a muscle biopsy to diagnose it?
Usually not. A diagnosis is typically made based on your medical history, symptoms, and functional tests like the timed chair rise. Blood tests (normal CK levels) and EMG (normal results) help rule out other conditions. A biopsy is only done if the diagnosis is unclear or if there’s suspicion of another muscle disease. In steroid myopathy, the biopsy would show type 2b fiber atrophy without inflammation - but this test is invasive and rarely needed.
Can I still exercise while on steroids?
Yes - but you need to choose the right kind. Light to moderate resistance training is not only safe, it’s essential. Avoid heavy lifting, high-intensity intervals, or long endurance sessions. Focus on controlled movements: squats, step-ups, resistance band rows, and wall push-ups. Always warm up first. If you feel unusual fatigue or soreness the next day, you’re pushing too hard. Less is more here.
How long does it take to recover from steroid myopathy?
Recovery varies. Some people notice small improvements in 4-6 weeks with consistent therapy. Full recovery usually takes 3-6 months. The speed depends on how long you’ve been on steroids, your starting strength, and how consistently you follow your rehab plan. Even if you can’t stop steroids, staying active helps prevent further loss and supports gradual regain.
Are there any supplements that help?
There’s no strong evidence that supplements like creatine or protein powders reverse steroid myopathy on their own. However, getting enough protein - about 1.2 to 1.6 grams per kilogram of body weight daily - supports muscle repair. Vitamin D deficiency is common in people on long-term steroids, so checking your levels and supplementing if low can help. Always talk to your doctor before adding supplements.
Can steroid myopathy affect breathing?
In severe or acute cases - especially with high-dose IV steroids in ICU patients - the muscles that help you breathe (like the diaphragm) can weaken. This happens in about 15-20% of critical care cases and may require temporary breathing support. For people on oral steroids for chronic conditions, respiratory muscle weakness is rare but possible. If you notice shortness of breath during normal activities, tell your doctor immediately.
What’s the difference between steroid myopathy and polymyositis?
Both cause proximal weakness, but they’re very different. Polymyositis is an autoimmune disease with muscle inflammation, elevated CK levels (often over 500 U/L), abnormal EMG, and sometimes fever or joint pain. Steroid myopathy has normal CK, no inflammation on biopsy, and no systemic symptoms. Crucially, polymyositis gets worse when you stop steroids, while steroid myopathy improves when you reduce them. Treatment is completely different: immunosuppressants for polymyositis, physical therapy for steroid myopathy.



Lu Jelonek
December 24, 2025 AT 21:46I never realized how quietly steroids could steal your strength. I’ve been on prednisone for lupus for six years, and it wasn’t until I couldn’t lift my granddaughter that I knew something was off. No pain, no swelling-just this slow fade. I wish I’d known about the chair test sooner. Thank you for writing this.
siddharth tiwari
December 25, 2025 AT 10:53they say steroids cause muscle loss but no one talks about how the pharma companies know this and still push it. they dont care if you cant stand up they just want you to keep buying. this is all profit driven. the real cure? stop taking it. but ofc theyll never say that.
Adarsh Dubey
December 25, 2025 AT 23:50This is one of the most practical and well-researched posts I’ve seen on steroid side effects. The functional tests are gold-simple, reliable, and overlooked. I’m a physio in Delhi and I’ve seen this exact pattern in COPD patients. We’ve started using the timed chair rise routinely now. It’s changed how we track progress. Also, the point about avoiding high-intensity work is critical. Too many patients try to ‘power through’ and end up injured.
claire davies
December 27, 2025 AT 03:05Oh my goodness, this hit me right in the chest. I’ve been on low-dose steroids for asthma since I was 12, and now I’m 41 and I can’t carry my own groceries without needing a rest. I thought I was just out of shape-turns out my muscles were quietly unraveling. The part about the dynamometer? That’s it. I’ve had so many doctors pat me on the head and say ‘you’re just getting older.’ But no, I’m not. I’m being medicated into weakness. I’m going to print this out and hand it to my rheumatologist tomorrow. Thank you for giving me the words I didn’t know I needed.
Raja P
December 28, 2025 AT 02:38good info. i’ve been on 10mg prednisone for 18 months and started doing bodyweight squats last month. barely any change yet but i feel a little more stable when i stand up. gonna keep at it. also agree with avoiding heavy lifting. my buddy tried deadlifts and ended up with lower back pain for weeks. not worth it.
Joseph Manuel
December 29, 2025 AT 06:30The assertion that steroid myopathy is underdiagnosed is statistically unsupported. The cited prevalence range (2.4%–21%) is too broad to be meaningful without stratification by dose, duration, and comorbidities. Furthermore, the claim that 78% of patients have deficits undetected by manual muscle testing lacks a reference to the original study. This article reads more like advocacy than evidence-based medicine.
Abby Polhill
December 30, 2025 AT 14:23Proximal weakness + normal CK + no pain = steroid myopathy. That’s the triad. And yes, the chair rise test is the unsung hero here. I’ve used it in my neuro clinic for years. Patients think they’re ‘just tired’-but when you time them, it’s obvious. The real tragedy? They’re often referred to rheumatology for ‘inflammatory myopathy’ when it’s just steroid damage. We need more PTs trained in this. Also-vamorolone? Yes. Please. We need alternatives.
Bret Freeman
December 30, 2025 AT 16:07THIS IS WHY I STOPPED STEROIDS. I WAS ON 40MG A DAY FOR A YEAR AND I COULDNT GET OFF THE FLOOR WITHOUT USING MY HANDS. MY DOCTOR SAID IT WAS ‘NORMAL.’ I SAID NO. I WENT OFF THEM ON MY OWN. TOOK 5 MONTHS BUT I GOT MY STRENGTH BACK. NOW I’M 100% OFF THEM AND I CAN DO PUSH-UPS AGAIN. DON’T LET THEM TELL YOU IT’S ‘JUST PART OF THE DISEASE.’ IT’S NOT. IT’S THE DRUG.
Austin LeBlanc
January 1, 2026 AT 02:36Why are you letting them poison you? If you’re on steroids long-term, you’re already losing your life to them. Why not fight harder? Why not switch to biologics? Why not go gluten-free, keto, alkaline diet, yoga, cryotherapy, and meditation? You’re choosing weakness. This isn’t medical advice-it’s surrender.
niharika hardikar
January 2, 2026 AT 15:28The clinical utility of the Gower’s maneuver in outpatient rheumatology settings is questionable due to lack of standardization in chair height and floor surface. Furthermore, the proposed rehabilitation protocol lacks specificity regarding eccentric loading parameters and does not account for concurrent osteoporosis, which is highly prevalent in this population. Without addressing bone density, resistance training may pose undue fracture risk.
EMMANUEL EMEKAOGBOR
January 2, 2026 AT 23:46Thank you for this. In Nigeria, many patients are told that weakness is just from the disease or age. We don’t have access to dynamometers or specialized physiotherapists. But we do have resistance bands and community health workers. I’ve started teaching the chair rise test to our local nurses. It’s simple, it’s free, and it saves dignity. I hope this spreads.
CHETAN MANDLECHA
January 4, 2026 AT 15:09My dad was on 60mg prednisone for 3 weeks in ICU after pneumonia. He couldn’t walk for months after. They never mentioned this. I had to Google it. This post should be mandatory reading for every ICU nurse and resident.
Jillian Angus
January 6, 2026 AT 05:47I started doing wall sits last week. It’s embarrassing but it’s something. I’m not strong yet but I’m trying. That’s all I’ve got.
Gray Dedoiko
January 6, 2026 AT 16:25Thank you for writing this. I’ve been on prednisone for 10 years and I thought I was just getting older. I didn’t realize I could fight back. I’m going to start the chair test every Sunday and log it. Maybe I’ll get my grandkids back.