Every year, tens of thousands of children accidentally swallow medications because they were left within reach. Seniors mix up pills because bottles look too similar. Insulin loses potency because it was left on the counter. These aren’t rare mistakes-they’re predictable results of poor storage habits. A home medication storage checklist isn’t just a good idea. It’s a life-saving system.
Where to Store Medications (And Where Not To)
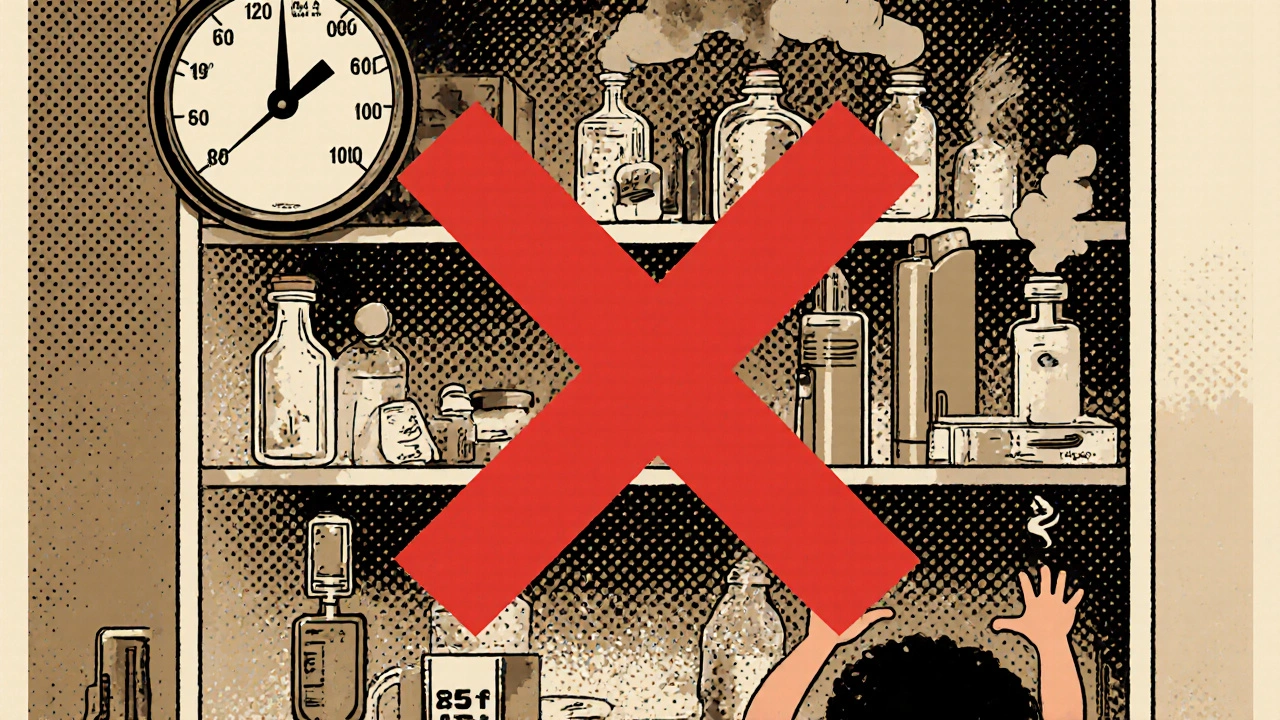
The bathroom cabinet is the worst place in your house for most medicines. It’s humid, hot during showers, and full of fluctuations. The temperature can jump 10-15 degrees when you turn on the shower, and humidity spikes to 80-90%. That’s enough to break down pills, creams, and inhalers faster than you think. Studies show medications stored in bathrooms degrade 30-50% faster than those kept in stable environments. Instead, pick a cool, dry, and consistent spot. A linen closet, a drawer in a bedroom dresser, or a powder room far from the shower works best. The ideal temperature range is 68-77°F, with humidity between 40-50%. Avoid windows, radiators, and the top of the fridge. If your home gets really hot in summer, consider a small, dedicated storage box inside a closet with a thermometer. Light matters too. Some medications-like nitroglycerin or certain antibiotics-break down when exposed to sunlight. Store these in their original amber bottles or inside an opaque container. Don’t just toss them into a clear plastic bin.Separate Medications by Person and Type
Mixing medications is one of the biggest causes of errors. If you have more than one person living in your home, keep their meds completely separate. Even if you think you know which bottle belongs to whom, stress, fatigue, or poor eyesight can lead to mistakes. Use different shelves, drawers, or labeled bins. Organize by route of administration too. Keep oral pills in one section, topical creams in another, inhalers in a third, and injectables in a fourth. Never store an eye drop next to a skin cream. The FDA documented over 120 cases between 2018 and 2020 where people accidentally used topical products as oral meds-some with serious results. High-alert medications like insulin, warfarin, and opioids need extra care. Store them in a separate locked container, clearly labeled “High Alert.” Even if you’re the only one taking them, this prevents confusion if someone else needs to help in an emergency.Lock It Down
Standard medicine cabinets don’t stop kids. Consumer Product Safety Commission tests show they block only 12% of access attempts. A 2023 study in Pediatrics found households using locked medicine lockboxes saw 92% fewer accidental ingestions in children under five. You don’t need a safe. A simple combination lockbox that mounts to a wall or bolts to a dresser works fine. Keep it at least four feet off the ground and behind three closed doors if possible. Kids who access meds usually do it in under 10 minutes-so make it hard to find and harder to open. If you have teens or someone in the house with a history of substance use, secure storage is even more critical. One in three teens who misuse prescription drugs get them from home cabinets. A locked box reduces that risk dramatically.
Track Expiration Dates Like a Pro
Most people don’t know their pills have expiration dates. Or worse-they think “expired” means “harmful.” The truth? Most medications stay effective for years past their printed date if stored properly. But potency drops. One FDA study found that after three years, only 42% of the original strength remains. Check your meds every six months. Set a reminder on your phone for the same time as daylight saving changes-spring forward, fall back. That’s when most people remember to update things anyway. Look for signs of degradation: pills that are cracked, discolored, or smell funny. Creams that separate or turn grainy. Inhalers that don’t spray right. If something looks or smells off, throw it out. Don’t risk it. For multi-dose vials-like insulin or eye drops-mark the date you opened them. Manufacturers say most are good for 14 to 56 days after opening, depending on the product. Write that date right on the bottle with a permanent marker.Special Cases: Insulin, Inhalers, and More
Insulin needs special handling. Unopened vials must stay refrigerated at 36-46°F. Once opened, they can stay at room temperature for up to six weeks, depending on the type. But never leave them in a hot car or near a stove. A 2022 American Diabetes Association study found 38% of users store in-use insulin incorrectly-cutting its effectiveness by up to 30%. Inhalers can malfunction if they get too cold or too hot. Store them at room temperature. Keep them in a small plastic box to prevent accidental button presses. If you use one daily, keep it next to your toothbrush-not in the medicine drawer-so you don’t forget it. Topical products like creams, lotions, and bug spray count as medications too. Under North Carolina’s Kaitlyn’s Law, these must be stored in original containers with labels. That’s true for all households, not just childcare settings. If the label’s missing, write the name, dose, and date on the container.
Dispose of Expired or Unused Meds Safely
Never flush pills down the toilet. That’s how pharmaceuticals end up in rivers and drinking water. A 2021 USGS study found traces of medications in 80% of U.S. waterways. Flushing leaves 60-80% of the drug intact. Use a drug take-back program. The DEA holds National Prescription Drug Take Back Days twice a year-in April and October. Over a million pounds of meds were collected in 2022 alone. Many pharmacies and police stations also offer year-round drop boxes. If there’s no take-back option nearby, mix pills with something unappetizing-used coffee grounds, kitty litter, or dirt-in a sealed plastic bag. Use a 1:3 ratio (one part meds, three parts filler). This makes them unattractive to kids or pets and prevents extraction. Put the bag in your regular trash.Build Your Checklist and Stick to It
Here’s your practical checklist. Print it. Tape it to your medicine storage area. Check it every six months.- Medications stored away from bathrooms, kitchens, and windows?
- Temperature between 68-77°F, humidity 40-50%?
- Light-sensitive meds in dark containers?
- Each person’s meds stored separately?
- Oral, topical, injectable, and inhalers in separate zones?
- High-alert meds (insulin, opioids, warfarin) in locked, labeled container?
- All meds in original containers with labels?
- Opened multi-dose items marked with date opened?
- Medications stored at least 4 feet high and behind locked doors?
- Lockbox used? Combination lock preferred over key?
- Expired meds identified and removed every 6 months?
- Disposal plan in place? Take-back location known?
Why This Works
A 2023 Consumer Reports survey of 2,500 households found that families using a formal storage checklist had 89% fewer medication errors than those who didn’t. That’s not magic. It’s structure. When you have a system, you don’t rely on memory. You don’t guess. You check. You label. You lock. You dispose. This isn’t just about safety. It’s about making sure your meds work when you need them. An expired antibiotic won’t cure an infection. Weak insulin won’t control blood sugar. A misread pill can send someone to the ER. Start small. Pick one thing from this checklist to fix this week. Maybe it’s moving your meds out of the bathroom. Or putting a lockbox on the top shelf. Do that. Then do the next one. Your family’s health depends on it-not on luck, not on hope. On a simple, clear, and consistent system.Can I store all my medications in one drawer?
No. Even if you’re the only person using them, storing all meds together increases the risk of mixing them up. Keep each person’s medications separate, and group them by type-oral, topical, injectable. Use dividers or small bins to avoid confusion.
What if I don’t have a lockbox?
Use a locked cabinet or closet that children can’t reach. If you have a small tool box or jewelry case with a key or combination lock, that works as a temporary solution. The goal is to make access difficult for kids, teens, or visitors. A simple lock, even if not medical-grade, is better than nothing.
Are expired medications dangerous to take?
Most expired meds aren’t toxic, but they lose potency. Taking an expired antibiotic could mean the infection doesn’t clear. Expired insulin may not lower blood sugar enough. If a pill looks cracked, smells odd, or a cream has changed texture, throw it out-even if it’s within the printed expiration date.
How often should I check my medication storage?
Do a full review every six months. Pair it with daylight saving time changes-it’s easier to remember. Check expiration dates, look for physical changes in pills or creams, and make sure everything is still in its proper place. Daily temperature checks are only needed for refrigerated meds like insulin.
Can I keep my medications in the fridge?
Only if the label says so. Most meds don’t need refrigeration. Storing them in the fridge can cause moisture damage or freezing, which ruins some formulations. Insulin and some liquid antibiotics must be refrigerated until opened. Keep them away from food and never store them in the door-temperatures swing too much there.
What should I do with old inhalers?
Don’t throw them in the trash or recycle bin. Many inhalers contain propellants that are harmful to the environment. Check with your pharmacy-they often have special disposal bins for inhalers. If not, contact your local hazardous waste facility. Never puncture or burn them.
Is it okay to store vitamins and supplements with prescription meds?
No. Vitamins, herbal supplements, and over-the-counter products should be stored with your other meds, but in a clearly labeled separate section. They’re still medications, and mixing them without clear labels increases the risk of accidental overdose or interaction.


Segun Kareem
November 17, 2025 AT 00:21Man, I never thought about how humidity kills meds until I saw my dad’s asthma inhaler go useless after a bathroom storage fail. Now I keep everything in a locked drawer in the bedroom-no more guessing games. This checklist? Print it. Tape it. Live by it. Your future self will thank you.
Also, side note: if you’re storing insulin in the fridge door? You’re doing it wrong. Temperature swings there are brutal. Stick it in the back, not the chaos zone.
Jessica M
November 17, 2025 AT 12:02It is imperative to underscore the clinical significance of adhering to recommended environmental parameters for pharmaceutical storage. The degradation kinetics of active pharmaceutical ingredients are demonstrably accelerated under conditions of elevated temperature and relative humidity, as corroborated by the United States Pharmacopeia (USP) Chapter 661 and the Food and Drug Administration’s Stability Guidelines.
Furthermore, the segregation of medications by patient and route of administration is not merely a best practice-it is a regulatory expectation within institutional settings and should be replicated in domestic environments to mitigate polypharmacy errors. The use of opaque, child-resistant containers for high-alert medications is not optional; it is a bioethical imperative.
Erika Lukacs
November 18, 2025 AT 18:08Interesting. So we’re now treating our medicine cabinets like nuclear launch codes? I mean, sure, it’s smart. But is it a little… excessive? At what point does safety become performance art?
I’m just saying-my grandma kept her pills in a cookie jar. She lived to 97. Maybe the real secret is not the lockbox, but the fact that she never took them on time anyway.
Rebekah Kryger
November 19, 2025 AT 02:54Okay but let’s be real-this whole ‘locked box’ thing is just corporate fearmongering wrapped in a wellness bow. The FDA says most drugs are still effective past expiration. So why are we being told to throw out perfectly good pills? Who benefits? Pharma? The lockbox manufacturers? The anxiety-inducing wellness industrial complex?
Also, ‘high-alert meds’? That’s just code for ‘we don’t trust you to not be an addict.’ I’ll keep my opioids in the same drawer as my Advil, thanks. I’m not a child.
Victoria Short
November 20, 2025 AT 00:39Ugh. I just moved. I have a pile of meds on my nightstand. I’ll get to it. Maybe next year.
Eric Gregorich
November 20, 2025 AT 12:44Have you ever sat in a silent room at 3 a.m. and stared at your insulin vial wondering if you’re doing enough? If you’re enough? If your body is a temple or just a broken machine that keeps asking for more pills? This checklist isn’t about storage-it’s about control. It’s about screaming into the void and hoping the void doesn’t swallow you whole.
I used to leave my pills on the counter because I was tired of being responsible. Then my brother overdosed on his own anxiety meds. He’s fine now. But I don’t sleep anymore. So I lock them. I label them. I check them. Every six months. Like a prayer.
This isn’t a guide. It’s a lifeline. And if you think that’s dramatic-you haven’t held someone’s hand while they stop breathing because a pill lost its strength.
Phil Best
November 22, 2025 AT 07:18Let’s be honest-this whole post reads like a pharmaceutical ad disguised as public service. ‘Lock it down!’ ‘Don’t store near windows!’ ‘Mark your expiration dates!’
Meanwhile, in the real world, people are choosing between rent and refilling prescriptions. You think they’ve got time to buy a $50 lockbox? Or label every pill? Or check humidity levels?
Here’s a radical idea: make meds affordable and accessible. Then worry about the storage. Until then, this is just virtue signaling for people who can afford to overthink their medicine cabinet.
Parv Trivedi
November 23, 2025 AT 20:02This is beautifully practical. I’ve shared this with my family in India-we have three generations living together, and medication mix-ups were becoming common. We’ve now assigned each person a color-coded bin, and my mother writes dates on bottles with a marker. Simple. Effective.
Also, thank you for mentioning disposal. So many people here flush pills because they don’t know better. Now I’ll take them to the pharmacy on my next visit. Small steps, big impact.