Fatty Meal Calculator for Medication Absorption
How Fatty Foods Help Medications
For lipid-based medications, you need 20-30 grams of dietary fat to ensure optimal absorption. Without sufficient fat, these medications may be ineffective. This calculator helps you determine if your meal meets the requirement.
Calculate Your Meal's Fat Content
Ever wonder why some pills come with instructions to take them with food-especially fatty food? It’s not just to avoid an upset stomach. For certain medications, eating fat isn’t optional-it’s part of how the drug works. Lipid-based medications rely on dietary fat to get into your bloodstream effectively. Without it, they might as well be useless.
Why Fat Matters for Some Drugs
Nearly 70% of new drugs being developed don’t dissolve well in water. These are called poorly water-soluble compounds, and they’re a major headache for drugmakers. If a drug can’t dissolve, your body can’t absorb it. That’s where fat comes in. Fatty foods trigger your body’s natural digestive processes that help dissolve and carry these drugs across the gut wall. When you eat fat, your body releases bile and digestive enzymes. These break down the fat into tiny droplets and mix them with the drug, trapping it in structures called micelles. Think of it like a soap bubble holding onto the drug so it can slip through your intestinal lining. Without this, the drug just sits there, unchanged, and gets flushed out. This isn’t theory-it’s proven. Take cyclosporine, a drug used after organ transplants. The original version, Sandimmune®, had wildly inconsistent absorption. Patients needed multiple doses a day and strict timing with meals. The newer lipid-based version, Neoral®, changed everything. It boosts bioavailability by 20-30% and lets people take it once or twice daily, regardless of what they ate. That’s not a small win-it’s life-changing for transplant patients.How Lipid-Based Formulations Work
Pharmaceutical companies don’t just tell you to eat a burger with your pill. They engineer the pill itself to work with fat. These are called lipid-based drug delivery systems. The most common type is called SEDDS-Self-Emulsifying Drug Delivery Systems. They’re tiny capsules filled with oil, surfactants, and solvents that turn into a milky liquid when they hit your gut. These systems use medium-chain triglycerides (MCTs), like those found in coconut oil. MCTs digest faster than long-chain fats from meat or butter. In just 15-30 minutes, they break down into components that help dissolve the drug and keep it suspended in your gut fluid. That’s three to five times longer than water alone can hold the drug in solution. The magic happens in your small intestine, where bile salt levels peak. That’s when these lipid droplets become super effective at carrying drugs into your blood. Studies show lipid-based versions of drugs like fenofibrate (used for cholesterol) can increase absorption by up to 31%. That means lower doses, fewer side effects, and more consistent results.Food Effect: The Real-World Impact
The term “food effect” sounds technical, but it’s simple: what you eat changes how well your medicine works. For some drugs, taking them on an empty stomach cuts absorption by half. For others, eating fat doubles it. Take itraconazole, an antifungal. The capsule version needs a fatty meal to work at all. Without it, only 20-30% of the drug gets absorbed. The lipid-based oral solution, Sporanox®, bypasses that problem. Even on an empty stomach, it delivers 2.8 times more drug into your blood. That’s why doctors now prefer the liquid form for serious fungal infections. But here’s the catch: not all drugs benefit. Drugs that dissolve easily in water (BCS Class I) don’t need fat. In fact, fat can slow them down by delaying stomach emptying. Same goes for drugs that need acid to dissolve-like some osteoporosis meds (bisphosphonates). Taking those with a fatty meal can make them less effective. Patients on lipid-based drugs often notice the difference. Reddit threads from people managing transplant rejection or high triglycerides say things like, “I don’t have to plan my meals around my pills anymore,” or “The stomach pain from the old version is gone.” That’s not placebo-it’s science.
Cost, Convenience, and Trade-Offs
Lipid-based formulations aren’t perfect. They’re more expensive. A 30-day supply of Sporanox® oral solution can cost $1,200. The generic capsule? Around $300. That’s a four-fold difference. Insurance doesn’t always cover the pricier version unless you’ve tried the cheaper one first. They’re also trickier to make. These drugs need special packaging-usually soft gelatin capsules that protect the oil from air and light. The manufacturing process takes 18-24 months to develop, compared to 12-15 for regular pills. That’s why only about 35% of new drugs for poorly soluble compounds now use this tech, up from 15% in 2015. And then there’s variability. If you have a digestive disorder-Crohn’s, celiac, or even long-term antibiotic use-your body might not produce enough bile or enzymes. That can wreck the whole system. Experts warn that lipid-based drugs aren’t one-size-fits-all. What works for one person might fail for another.What’s Next? Smart Capsules and Personalized Dosing
The future of lipid-based delivery is getting smarter. Researchers at MIT recently tested a “smart lipid capsule” that senses pH and enzyme levels in your gut and releases the drug only when conditions are right. It’s still in early testing, but early results show it could eliminate food effect variability entirely. Another breakthrough came in March 2023 with Matinas BioPharma’s LNC platform. Their antifungal drug, amphotericin B, hit 92% bioavailability in trials-compared to just 30% with the old version. That’s a game-changer for patients with life-threatening fungal infections who couldn’t tolerate the toxic side effects of traditional treatments. The FDA and EMA now require drugmakers to test food effects rigorously. That means more labels will clearly say “take with food” or “take on empty stomach.” You’ll see this more often, especially with new cancer, antiviral, and immune drugs.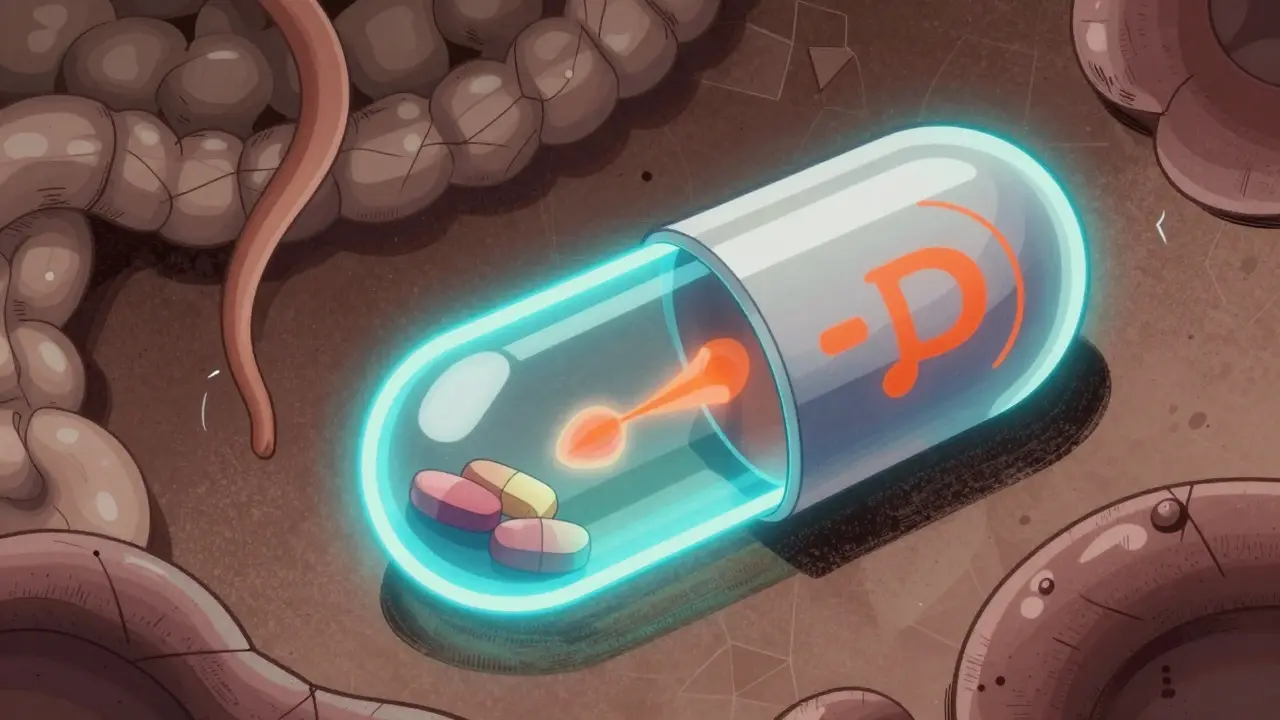
What You Should Do
If you’re on a medication that’s known to have a food effect, don’t guess. Check the label. Ask your pharmacist. Don’t assume “with food” means any snack. For lipid-based drugs, you need actual fat-avocado, nuts, olive oil, eggs, cheese. A banana won’t cut it. If you’re switching from a generic to a lipid-based version, give it time. Your body might respond differently. Track how you feel, your side effects, and whether your symptoms improve. Many patients report fewer stomach issues and more consistent energy levels. And if cost is a barrier, ask about patient assistance programs. Some manufacturers offer discounts or free samples. Generic versions aren’t always inferior-but for lipid-based drugs, they often are.Bottom Line
Fatty foods aren’t just calories-they’re delivery vehicles. For nearly half of all new drugs, fat is the missing piece that turns a weak medicine into a powerful one. Lipid-based formulations turn your body’s natural digestion into a drug-enhancing tool. It’s not magic. It’s pharmacology working with biology, not against it. The next time your doctor says, “Take this with a meal,” don’t just nod. Ask: What kind of meal? And why? You might just be holding the key to better results.Do all medications need to be taken with fatty foods?
No. Only medications designed for lipid-based delivery or those with poor water solubility benefit from fat. Drugs like antibiotics, blood pressure pills, or most pain relievers don’t need it. Always check your prescription label or ask your pharmacist. Taking a drug with fat when it’s not needed can reduce its effectiveness or cause side effects.
What counts as a "fatty meal" for drug absorption?
A meal with at least 20-30 grams of fat is typically enough. Examples include two eggs with cheese, a tablespoon of olive oil on vegetables, a handful of almonds, or a serving of salmon. A slice of pizza or a burger with fries also works. Avoid low-fat snacks like fruit, rice cakes, or yogurt-these won’t trigger the necessary digestive response.
Can I take lipid-based medications with a smoothie or protein shake?
Only if the smoothie contains added fat. A fruit-and-protein-powder shake with no oil, nut butter, or avocado won’t help. But if you add a spoon of peanut butter, flaxseed oil, or full-fat yogurt, it can be effective. The key is triggering bile release, which requires real dietary fat-not just calories or protein.
Why are lipid-based drugs more expensive?
They require complex manufacturing, specialized ingredients like MCTs and surfactants, and protective packaging (usually soft gel capsules). Development takes longer and involves more testing. A lipid-based formulation can cost 25-35% more to produce than a standard tablet. That cost gets passed on, especially if there’s no generic version available yet.
Do lipid-based medications work the same for everyone?
Not always. People with conditions like Crohn’s disease, cystic fibrosis, or gallbladder removal may not produce enough bile to activate the system. Older adults and those on long-term antibiotics can also have reduced fat digestion. If you notice your medication isn’t working as well, talk to your doctor-your body’s ability to process fat might be part of the issue.
Are there natural alternatives to lipid-based drug formulations?
No. While eating fat helps absorption, you can’t replace a lipid-based drug formulation with diet alone. These formulations are precisely engineered to dissolve and carry the drug at the right time and place. Eating avocado with a regular pill won’t turn it into a lipid-based drug. The science is in the formulation-not just the food.


