When you eat a meal and still feel bloated, gassy, or like your stomach is sitting like a rock hours later, it’s easy to blame the food. But sometimes, the problem isn’t what you ate - it’s whether your body can break it down at all. Digestive enzymes are the body’s natural tools for turning food into usable nutrients. When they’re missing or not working right, symptoms like diarrhea, fatty stools, or constant indigestion can follow. For some people, enzyme supplements aren’t just a quick fix - they’re a necessary part of daily life. For others, they offer little to no help. Knowing the difference matters.
What Digestive Enzymes Actually Do
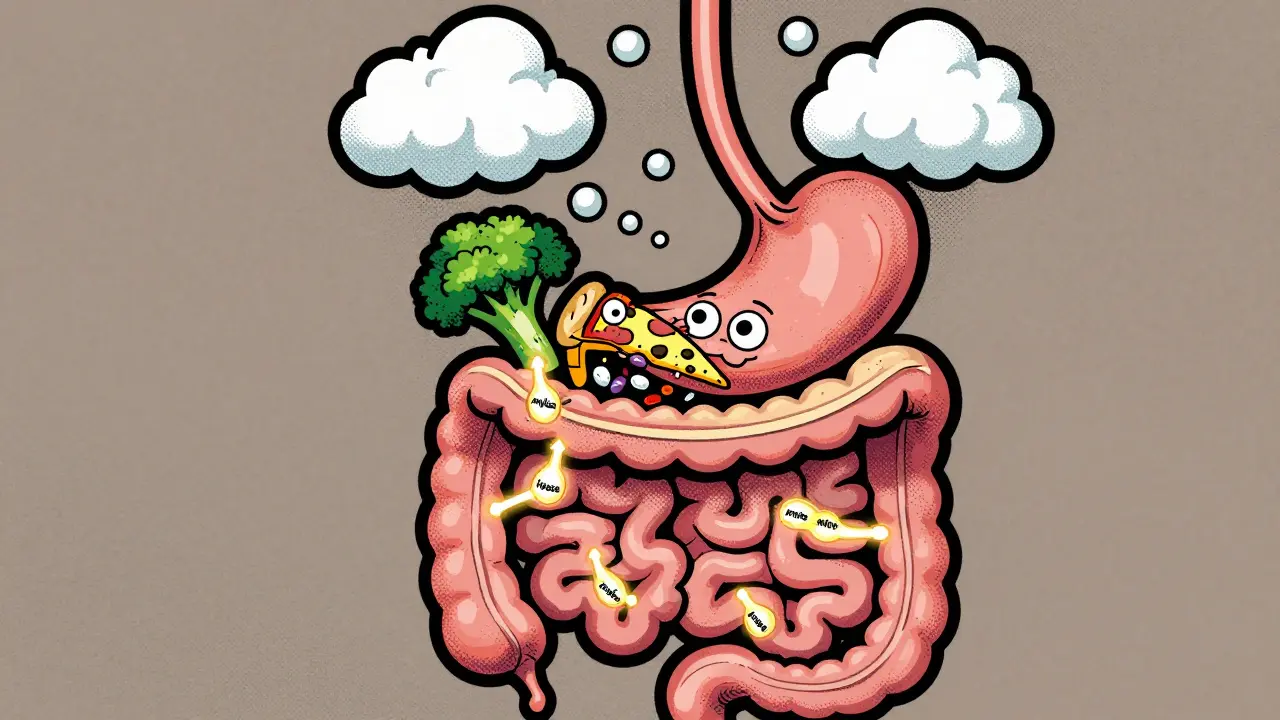
Your body makes enzymes every day - mostly in the pancreas. These include amylase for carbs, protease for proteins, and lipase for fats. Together, they break down your food so your intestines can absorb vitamins, minerals, and energy. Without enough of them, undigested food moves into the colon, where bacteria feast on it and produce gas, bloating, and loose stools. This isn’t just discomfort - it can lead to serious nutrient deficiencies over time.When Enzyme Supplements Are Medically Necessary
The clearest case for enzyme supplements is exocrine pancreatic insufficiency (EPI). This happens when the pancreas can’t produce enough enzymes. It’s common in people with chronic pancreatitis, cystic fibrosis, or after pancreatic surgery. About 30-50% of chronic pancreatitis patients have EPI, and up to 90% of those with pancreatic cancer do. Left untreated, EPI causes weight loss, malnutrition, and vitamin deficiencies - especially in fat-soluble vitamins like A, D, E, and K. Prescription enzyme replacement therapy (PERT), like Creon or Zenpep, is the gold standard here. These aren’t regular supplements - they’re FDA-approved drugs. Each capsule contains precise amounts of lipase, protease, and amylase, coated to survive stomach acid and release in the small intestine. Studies show PERT reduces fatty stools by 70-85% in EPI patients. For these people, enzyme supplements aren’t optional - they’re life-changing.OTC Enzymes: Helpful or Hype?
Over-the-counter (OTC) digestive enzymes are everywhere. Shelves at pharmacies and online stores are packed with blends promising relief from bloating, gas, and indigestion. But most aren’t designed for EPI. They’re marketed for general digestive discomfort - often targeting people with IBS, lactose intolerance, or sensitivity to beans and broccoli. Here’s the truth: OTC enzymes can help in specific cases. Lactase supplements, like Lactaid, work well for lactose intolerance. A 2021 meta-analysis found they reduce symptoms in about 50-60% of users. Enzymes that break down FODMAPs - like those in Digestive Gold - may help some IBS patients manage gas and bloating after high-FODMAP meals. But results vary. One study found 41% of IBS users stopped taking OTC enzymes within three months because they didn’t notice a difference. The bigger issue? Quality. Unlike prescription enzymes, OTC products aren’t regulated as drugs. A 2019 analysis found 20-30% of OTC supplements have inconsistent enzyme levels. ConsumerLab testing showed 15-25% contain less than 80% of what’s listed on the label. You might pay $25 a month for a bottle, but you could be getting barely any active enzyme at all.
Prescription vs. OTC: The Real Differences
| Feature | Prescription PERT (e.g., Creon) | OTC Enzymes (e.g., NOW Foods, Enzymedica) |
|---|---|---|
| Enzyme Source | Porcine (pig-derived) | Microbial (fungus/bacteria) or plant-based |
| Lipase per Dose | 10,000-40,000 units | 10,000-20,000 units |
| Enteric Coating | Yes - survives stomach acid | Usually no |
| Dosing Precision | Standardized, FDA-regulated | Variable, inconsistent between batches |
| Effectiveness for EPI | 70-85% symptom reduction | 30-40% or less |
| Effectiveness for IBS/Lactose | Effective but not typically used | 50-60% symptom reduction in some users |
| Cost per Dose | $1.50-$3.00 (often covered by insurance) | $0.50-$1.00 |
| Regulation | FDA-approved drug | Dietary supplement (less oversight) |
Who Should Avoid Enzyme Supplements
Not everyone benefits - and some people can get worse. If you have acute pancreatitis, enzyme supplements are contraindicated. They can trigger flare-ups. Also, if you’re on proton pump inhibitors (PPIs) like omeprazole, your stomach acid is suppressed. That can stop enzymes from activating properly, especially non-enteric coated ones. Some users report constipation or even bezoars - undigested food clumps - from taking too much enzyme without matching it to meal size. Another red flag: people with SIBO (small intestinal bacterial overgrowth). Enzymes can feed the overgrown bacteria, making bloating and gas worse. If you’ve tried enzymes and felt worse, it’s worth getting tested for SIBO before continuing.How to Use Them Right
If you’re going to try enzymes, timing and dosage matter. Taking them after your meal is too late. You need to take them 10-15 minutes before eating so they’re ready when food hits your small intestine. For meals high in fat - like pizza or fried chicken - you’ll need more lipase. A general rule: 500 lipase units per gram of fat. A tablespoon of olive oil (14g fat) needs about 7,000 units. Start low. Begin with 10,000 lipase units per meal. Wait a week. If symptoms persist, increase by 10,000 units. Most people find their sweet spot between 25,000 and 50,000 units per meal. Never go above 80,000 units without medical supervision. Splitting your dose - taking half before the meal and half halfway through - helps if you eat slowly. One 2018 trial found this boosted symptom control by 35%.
What the Experts Say
Dr. Russell Havranek, a gastroenterologist with 15 years of clinical experience, says OTC enzymes are often his first recommendation for IBS patients - especially those with gas and bloating after meals. He’s seen consistent results with brands like Digestive Gold. But he’s quick to add: “If symptoms don’t improve in two weeks, it’s not the enzymes. It’s something else.” The American Gastroenterological Association is clear: PERT is strongly recommended for EPI. For everything else - IBS, functional dyspepsia, “leaky gut” - there’s insufficient evidence. And while some OTC enzymes may help, many marketing claims - weight loss, detox, energy boosts - are unsupported. A 2020 FDA analysis found 78% of OTC enzyme ads made claims with no clinical backing.Real Stories, Real Results
On Reddit, users with EPI say PERT gave them back their lives. One wrote: “I lost 40 pounds in six months before starting Creon. After one month, I gained 15 back - not from overeating, just because my body finally absorbed food.” Others with lactose intolerance swear by Lactaid. On Target.com, it has over 8,000 reviews with 82% saying they can now eat dairy without symptoms. But many IBS sufferers report disappointment. One Amazon reviewer said: “I took these with every meal for a month. Still bloated. Still gassy. Felt like I wasted $30.”What’s Next
New research is exploring enzyme blends tailored to individual microbiomes. Companies are testing combinations of enzymes and probiotics for IBS. A 2023 trial showed lactase plus Bifidobacterium reduced symptoms 45% more than lactase alone. Another study found gluten-specific enzymes reduced gluten toxicity by 80% in celiac patients - potentially offering a safety net for accidental exposure. But for now, the message stays simple: If you have EPI, get tested and use prescription enzymes. If you have IBS or lactose intolerance, try OTC enzymes - but choose reputable brands, start low, and give it two weeks. If nothing changes, don’t keep buying bottles. See a doctor. Your gut deserves better than guesswork.Can digestive enzymes help with IBS?
Yes, for some people. OTC enzyme supplements containing proteases, amylases, and lipases may reduce bloating and gas after high-FODMAP meals. Studies show about 50-60% of IBS patients experience symptom relief, but results vary. If you don’t notice improvement within two weeks, the enzymes likely aren’t the solution - and you should look into other causes like SIBO or food intolerances.
Are prescription digestive enzymes better than over-the-counter ones?
For exocrine pancreatic insufficiency (EPI), yes - by a large margin. Prescription enzymes like Creon have standardized, high-dose enzyme content with enteric coating to survive stomach acid. OTC products lack this precision and often don’t reach the small intestine intact. For EPI, OTC enzymes are ineffective in most cases. For general bloating or lactose intolerance, OTC enzymes can be just as helpful - if they contain the right enzymes in sufficient amounts.
Do digestive enzymes help with weight loss?
No. There’s no credible evidence that digestive enzymes promote weight loss. Many supplements market this claim, but it’s misleading. Enzymes help break down food - they don’t burn fat or speed up metabolism. Weight loss requires calorie control and physical activity. If a product claims otherwise, it’s likely violating FDA guidelines.
Can I take digestive enzymes with proton pump inhibitors (PPIs)?
It’s complicated. PPIs reduce stomach acid, which can interfere with how well some enzymes activate - especially non-enteric coated OTC products. Prescription PERT is designed to work even with low acid, but mixing PPIs and enzymes without medical guidance isn’t advised. If you’re on PPIs and still have symptoms, talk to your doctor before adding enzymes.
How do I know if I have exocrine pancreatic insufficiency (EPI)?
Symptoms include fatty, oily stools that float, unexplained weight loss, bloating, and nutrient deficiencies (like low vitamin D or B12). Diagnosis requires a fecal elastase-1 test - a simple stool sample that measures pancreatic enzyme levels. If levels are below 200 mcg/g, EPI is likely. If you have chronic pancreatitis, cystic fibrosis, or have had pancreatic surgery, you should be tested even if symptoms are mild.
Why do some people feel worse after taking digestive enzymes?
One common reason is undiagnosed SIBO (small intestinal bacterial overgrowth). Enzymes break down food into simple sugars and fats, which feed the excess bacteria in the small intestine, leading to more gas and bloating. Another reason is taking too high a dose, especially without matching it to meal fat content. Some people also react to fillers or additives in low-quality supplements. If symptoms worsen, stop taking them and consult a doctor.


Ambrose Curtis
January 27, 2026 AT 23:06Man, I tried those OTC enzyme pills for months after my pizza bloat crisis. Felt like i was throwing cash down the toilet. Then my doc ran the fecal elastase test and boom - EPI. Creon changed my life. No more floating turds, no more losing 2 lbs a week. I gained 18 lbs in 3 months just from eating like a normal human. Don’t waste your money on cheap stuff if you’re really struggling - get tested.