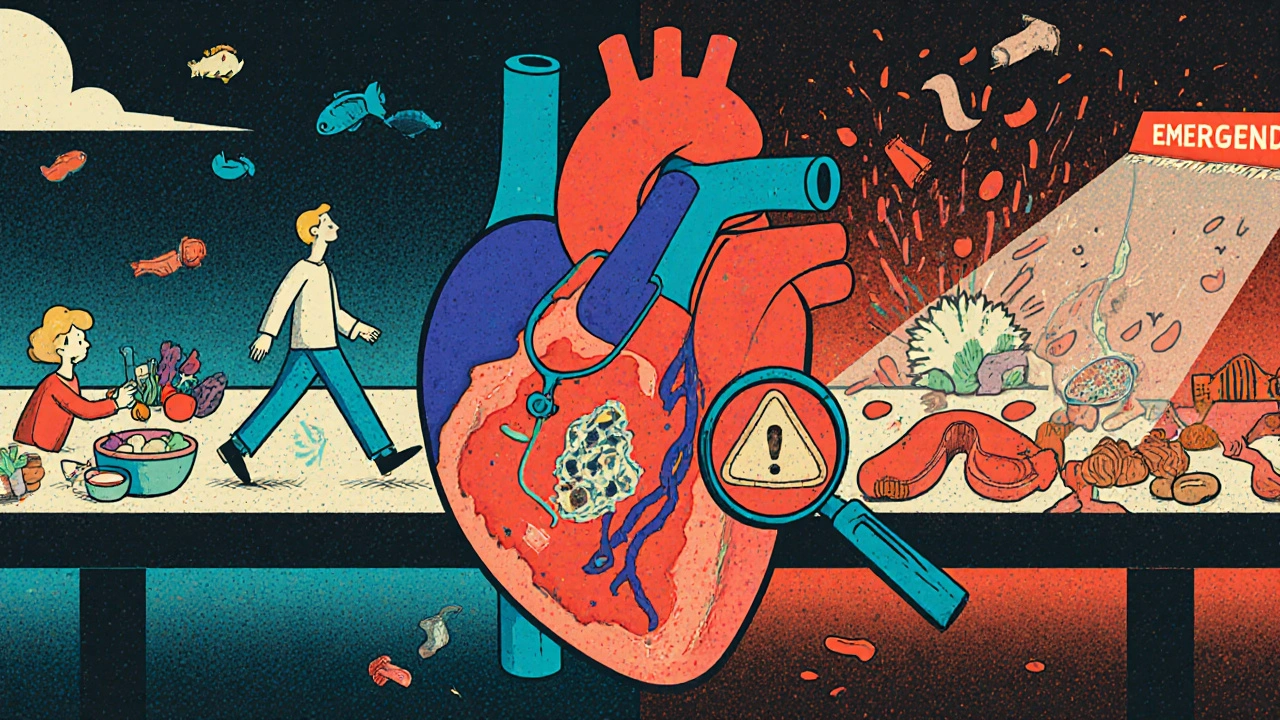
Coronary artery disease (CAD) isn't just a slow clog in the pipes-it’s a silent, ticking time bomb in your chest. Every year, over 360,000 people in the U.S. alone die from it. Globally, it’s responsible for 13% of all deaths. And here’s the thing: most people don’t realize they have it until something serious happens. That’s because CAD starts quietly, with fatty deposits building up over decades, often without symptoms. By the time chest pain shows up, the damage may already be advanced.
What Is Atherosclerosis, Really?
Atherosclerosis is the root cause of coronary artery disease. It’s not just cholesterol clogging your arteries-it’s a complex, active process inside the artery walls. Low-density lipoprotein (LDL), often called "bad cholesterol," slips into the lining of your arteries. Your immune system sends in white blood cells to clean it up. But instead of cleaning, they turn into foam cells, triggering inflammation. Over time, smooth muscle cells and fibrous tissue build up around this mess, forming a plaque.
Not all plaques are the same. Some are stable-thick, fibrous caps over a smaller lipid core. These can narrow the artery by more than 50%, causing predictable chest pain during exercise. Others are unstable: thin caps, big fatty cores, packed with inflammatory cells. These don’t always narrow the artery much-sometimes less than 50%-but they’re dangerous because they can rupture without warning. When they do, a blood clot forms on the spot, blocking blood flow completely. That’s when a heart attack happens.
This is why two people with the same level of artery narrowing can have totally different outcomes. One might have stable angina and live for years. The other could have a sudden cardiac event from a plaque that looked harmless on a scan.
Who’s at Risk? The Real Culprits Behind CAD
It’s easy to blame genetics or bad luck, but the biggest risk factors for CAD are mostly within your control. The 2023 ACC/AHA guidelines break risk into three levels: low (<1% chance of heart attack or death per year), intermediate (1-3%), and high (>3%). Most people who have heart attacks fall into the high-risk group.
Here’s who’s most at risk:
- Smokers: Smoking damages the artery lining, speeds up plaque buildup, and makes blood more likely to clot. Even occasional smoking raises your risk.
- People with diabetes: High blood sugar eats away at blood vessels. Diabetics are two to four times more likely to develop CAD than non-diabetics.
- Those with high LDL cholesterol: Levels above 160 mg/dL significantly increase risk. But even levels between 130-159 mg/dL can be dangerous if other risks are present.
- People with high blood pressure: Consistently above 130/80 mmHg puts extra strain on arteries, making them more prone to damage.
- Individuals with obesity: Especially with belly fat (waist over 40 inches for men, 35 for women). Fat tissue releases inflammatory chemicals that worsen atherosclerosis.
- Those with a history of heart attack, bypass surgery, or stents: Once you’ve had one event, your risk of another skyrockets.
- People with chronic kidney disease: An eGFR below 60 ml/min is a red flag. Kidney function and heart health are deeply linked.
Here’s something surprising: nearly 75% of first heart attacks happen in people classified as high-risk. Yet, many of these people aren’t even on the right medications. Risk isn’t just about numbers-it’s about patterns. If you have two or more of these risk factors, your chances of a major event jump dramatically.
How Is CAD Diagnosed? Beyond the Chest Pain
Many people assume chest pain is the only sign of CAD. But it’s not that simple. Some have no pain at all-especially women, older adults, and diabetics. Instead, they might feel tired, short of breath, or have nausea during activity. That’s why diagnosis isn’t just about symptoms.
Doctors use a mix of tools:
- Electrocardiogram (ECG): This quick, painless test checks your heart’s electrical activity. It can spot signs of past heart damage or current strain.
- Stress tests: You walk on a treadmill or ride a stationary bike while your heart is monitored. If your heart doesn’t get enough blood during exertion, it shows up as abnormal patterns.
- Coronary angiography: The gold standard. A thin tube is threaded into your artery, dye is injected, and X-rays show exactly where blockages are. It’s invasive, but often necessary before treatment.
- Ankle-Brachial Index (ABI): This simple test compares blood pressure in your ankle to your arm. If it’s low, it means you likely have plaque in your leg arteries too-which almost always means you have it in your heart arteries as well.
Recent guidelines also recognize "ischemia with nonobstructive coronary arteries" (INOCA). This means you have heart symptoms and reduced blood flow, but no major blockages on angiography. It’s real, it’s common, and it’s often overlooked. In these cases, tiny vessel disease or endothelial dysfunction is the culprit.
Treatment: It’s Not Just Pills and Surgery
There’s no magic bullet. Effective CAD treatment combines lifestyle changes, medications, and sometimes procedures-all tailored to your risk level.
Lifestyle is the foundation. No pill works as well as quitting smoking, eating real food, and moving daily. The Mediterranean diet-rich in olive oil, fish, nuts, vegetables, and whole grains-has been shown to reduce heart events by up to 30%. Walking 30 minutes a day, five days a week, cuts your risk of dying from CAD by nearly half.
Medications are non-negotiable for most. Here’s what’s typically prescribed:
- Statins: Lower LDL cholesterol and stabilize plaques. Even if your LDL is "normal," statins are often still recommended for high-risk patients.
- Aspirin: Used for secondary prevention (after a heart attack or stent). Not routinely recommended for primary prevention unless you’re very high risk.
- ACE inhibitors or ARBs: Help lower blood pressure and reduce heart strain, especially if you have diabetes or heart failure.
- Beta-blockers: Slow your heart rate, lower blood pressure, and reduce oxygen demand on the heart. Often used after a heart attack.
- SGLT2 inhibitors and GLP-1 agonists: Originally for diabetes, these drugs now show strong heart protection-even in people without diabetes.
Procedures: When and Why
- Percutaneous Coronary Intervention (PCI): A balloon is inflated to open a blocked artery, then a stent is placed to keep it open. Best for sudden blockages or severe angina. Not always needed for stable disease.
- Coronary Artery Bypass Grafting (CABG): A surgeon takes a blood vessel from your leg or chest and reroutes blood around the blockage. Recommended for multi-vessel disease, especially if you have diabetes.
Here’s the key: PCI doesn’t extend life in stable CAD. It only helps with symptoms. CABG, however, can improve survival in complex cases. The decision isn’t about what’s available-it’s about what’s right for your risk profile.
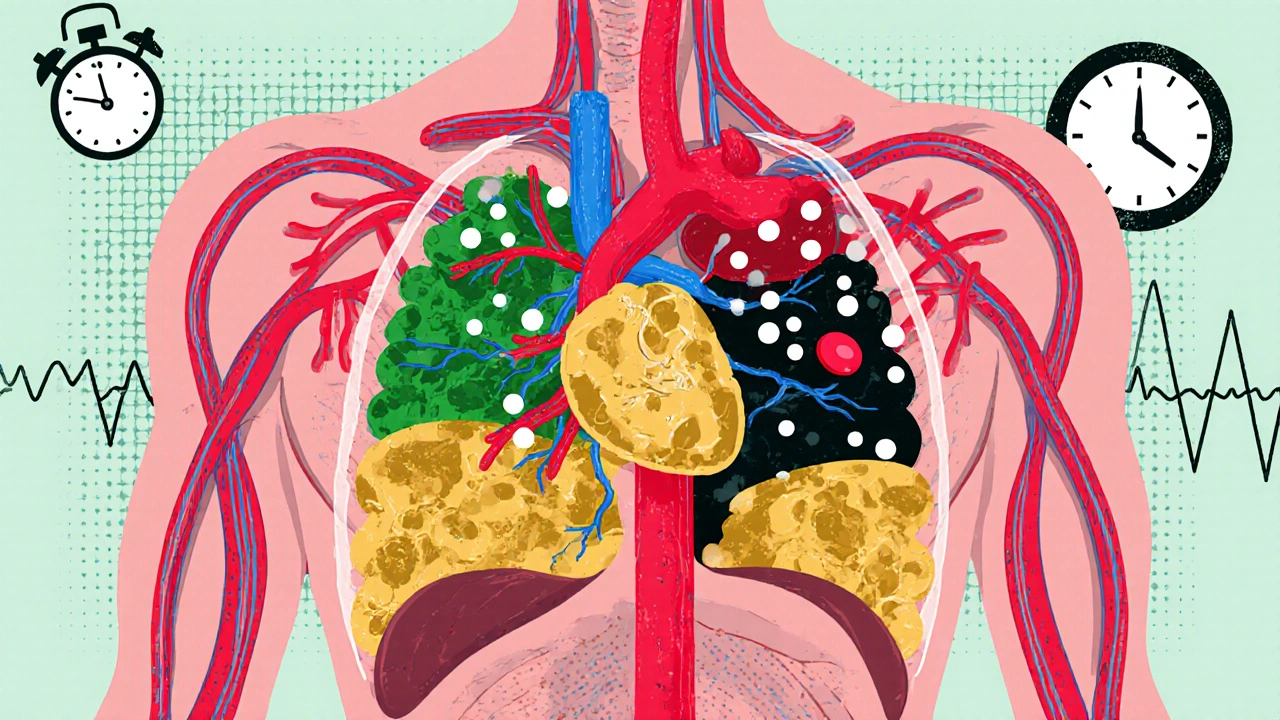
The New Frontier: Cardio-Oncology and Personalized Care
As more people survive cancer, we’re seeing more overlap. Chemotherapy and radiation can damage the heart. At the same time, heart disease patients are living longer with chronic conditions. That’s why cardio-oncology is growing fast-a field focused on managing both heart disease and cancer together.
Also, treatment is becoming more personalized. The 2023 guidelines stress that risk assessment isn’t just a number. It’s about your age, gender, family history, kidney function, inflammation markers, and even your mental health. Stress and depression are now recognized as independent risk factors for heart events.
Future treatments are looking at ways to stabilize plaques before they rupture-using drugs that target inflammation, not just cholesterol. Trials are underway for therapies that reduce plaque volume or change its composition. For now, the best tool we have is early detection and consistent management.
What You Can Do Today
If you’re worried about CAD, don’t wait for symptoms. Start with these steps:
- Get your blood pressure, cholesterol, and blood sugar checked-especially if you’re over 40 or have a family history.
- If you smoke, quit. Even one cigarette a day raises your risk. Support programs and nicotine replacement work.
- Move more. You don’t need to run a marathon. Aim for 150 minutes of brisk walking a week.
- Eat more plants. Swap processed snacks for nuts, fruit, or veggies. Cook with olive oil instead of butter.
- Ask your doctor about your risk score. Don’t just accept "you’re fine"-ask: "Am I low, medium, or high risk? What should I be doing differently?"
Coronary artery disease isn’t a death sentence. It’s a chronic condition-and like diabetes or high blood pressure-it can be managed. The difference between living well and facing a heart attack often comes down to one thing: acting before it’s too late.
Can you reverse coronary artery disease?
You can’t completely erase plaque, but you can stabilize it and even reduce its size. Aggressive lifestyle changes-like the Ornish or Mediterranean diets combined with daily exercise and stress management-have been shown to shrink plaque in studies. Statins also help by lowering LDL and reducing inflammation. The goal isn’t to make arteries perfectly clean-it’s to prevent rupture and blockage.
Do I need a stent if I have chest pain?
Not always. If your chest pain happens only with exertion and goes away with rest, you likely have stable angina. In that case, medications and lifestyle changes are the first-line treatment. Stents are usually reserved for when symptoms don’t improve with meds, or if tests show a severe blockage threatening heart muscle. For stable CAD, stents don’t extend life-they just relieve symptoms.
Can young people get coronary artery disease?
Yes. While CAD is more common after 50, plaque starts building in your 20s and 30s. With rising obesity, diabetes, and smoking rates in younger adults, heart attacks are now happening in people as young as 30. Genetics can play a role, but lifestyle is the biggest driver. If you have a family history and unhealthy habits, you’re at risk-even if you feel fine.
Is heart disease hereditary?
Having a close relative who had heart disease before age 55 (for men) or 65 (for women) increases your risk. But genes don’t determine your fate. Even with a strong family history, you can lower your risk significantly by controlling blood pressure, cholesterol, weight, and avoiding smoking. Genetics loads the gun-lifestyle pulls the trigger.
What’s the difference between stable and unstable angina?
Stable angina happens predictably-during exercise or stress-and goes away with rest or nitroglycerin. It’s caused by a fixed, narrow blockage. Unstable angina comes on suddenly, even at rest, lasts longer, and doesn’t fully resolve with rest or medication. It signals a ruptured or nearly blocked plaque and is a medical emergency. If you experience this, call for help immediately.
What Comes Next?
If you’ve been diagnosed with CAD, your next step isn’t panic-it’s planning. Work with your doctor to understand your risk level. Get a full lipid panel, check your kidney function, and ask about inflammation markers like hs-CRP. Don’t skip follow-ups. Many people start meds, feel better, and stop taking them. That’s when things go wrong.
If you haven’t been diagnosed but have risk factors, don’t wait for symptoms. Talk to your doctor about screening. A simple ABI test or stress test might be all you need to catch early disease. Prevention isn’t optional-it’s the most powerful treatment we have.

Pallab Dasgupta
November 22, 2025 AT 02:06Man, I read this and immediately thought of my uncle in Delhi-he smoked two packs a day, ate fried samosas for breakfast, and still claimed he was "fine" until he dropped in the grocery store. CAD doesn't care if you're tough or Indian or "used to it." It just waits. And when it hits? Boom. No second chances.
But here's the good part: my cousin reversed his plaque with just diet, walking 5K every morning, and quitting cold turkey. No stent. No drama. Just discipline. You can beat this. Not because you're lucky-because you choose to fight.
Stop waiting for symptoms. Start checking your numbers. Your future self will thank you.
And yes, I'm talking to you, uncle.
Ellen Sales
November 22, 2025 AT 05:46It's funny-how we treat our hearts like they're just a pump, not a living, breathing, feeling part of us. We stress, we sleep poorly, we eat garbage, and then we get mad when our body rebels. But the heart doesn't scream-it whispers. And we keep turning up the volume on our phones instead of listening.
Statins aren't magic. Neither are stents. The real medicine? Quiet mornings. Walking without headphones. Cooking with olive oil instead of rage. Loving yourself enough to show up for your body, even when it's boring. Even when no one's watching.
You don't need a diagnosis to start healing. You just need to care enough to begin.
Josh Zubkoff
November 23, 2025 AT 05:15Let’s be real-this whole article is just Big Pharma’s PR campaign wrapped in a lab coat. Statins? They cause diabetes, muscle atrophy, memory loss-you think your doctor knows this? Nah. They get kickbacks from pharma reps who bring free lunches and branded pens. And don’t even get me started on the "Mediterranean diet"-olive oil is expensive, and most people can’t afford it unless they’re living in a gated community in Santa Monica.
Meanwhile, the real cause of CAD? Environmental toxins, glyphosate in our food, 5G radiation, and the fact that we’re all being slowly poisoned by the government’s secret agenda to control us through heart disease. The FDA doesn’t want you to know that saturated fat is actually healthy-until they ban butter and call it a public health threat. Watch your back.
And don’t trust any doctor who says "just take aspirin." They’re not your friend. They’re a cog in the machine.
fiona collins
November 23, 2025 AT 19:48Thank you for this. Clear. Necessary. No fluff.
Check your numbers. Move daily. Eat real food. Quit smoking. Talk to your doctor. That’s it.
Not sexy. Not viral. But it works.
Rachel Villegas
November 24, 2025 AT 00:38I’ve been on a statin for five years. My LDL dropped from 178 to 72. I didn’t feel any different. No energy boost. No weight loss. No miracle. But I take it anyway. Because I’ve seen what happens when you don’t. My dad had a heart attack at 58. He thought he was fine too.
This isn’t about feeling good. It’s about not dying before your kids graduate college.
And yes, I eat kale. No, I don’t like it. But I eat it anyway.
giselle kate
November 24, 2025 AT 18:56America’s heart disease problem? It’s because we let immigrants and lazy people eat carbs and sit on couches all day. We used to be strong. We used to work. Now we’re a nation of people who think a 10-minute walk counts as exercise. Meanwhile, real men used to build things, lift weights, and eat bacon. Now we’re told to eat quinoa and cry about inflammation.
Stop blaming genetics. Stop blaming cholesterol. Blame the weak mindset. The weak culture. The weak government that tells you to take pills instead of standing up and moving.
If you want to live, stop whining. Get off the couch. Lift something heavy. Eat meat. Stop being afraid of fat.
It’s not complicated. It’s just hard. And most people aren’t hard enough.
Emily Craig
November 25, 2025 AT 09:28So let me get this straight-you’re telling me the best way to avoid a heart attack is to eat like a French peasant, walk like a grandma, and take pills that make me feel like a zombie?
And you wonder why people just… give up?
Look, I get it. I’m not saying this is easy. But if your doctor handed you a pamphlet titled "How to Be Alive in 2025" and it just said "eat veggies and don’t smoke," you’d laugh in their face. And honestly? You’d be right.
Because this system is broken. We treat symptoms like they’re the problem, not the warning signs. We medicate instead of heal. We measure LDL like it’s a GPA and forget that people aren’t lab rats.
But hey-at least we’ve got apps to track our avocado toast intake. Progress?
Karen Willie
November 26, 2025 AT 23:39I work in a clinic and see this every day. People come in scared, confused, overwhelmed. They don’t know where to start. So I tell them one thing: pick one thing. Just one.
Maybe it’s swapping soda for water. Maybe it’s walking around the block after dinner. Maybe it’s asking your doctor about your hs-CRP.
Don’t try to fix everything at once. You’ll burn out. Just start. Then come back tomorrow. And the next day.
Healing isn’t a race. It’s a rhythm. And you’re already on the right path just by reading this.
Leisha Haynes
November 28, 2025 AT 23:29So I went to my doctor last week and asked about my risk score. He said, "You’re fine. You’re young."
I’m 42. I have prediabetes. My waist is 38 inches. My dad had a triple bypass at 52.
"You’re fine."
Okay.
So I got my own lipid panel. LDL was 168. My doctor didn’t even mention it.
Turns out, "you’re fine" is just code for "I don’t have time to explain why you might die before 60."
Thanks, healthcare system. You’re a real gem.
Shivam Goel
November 29, 2025 AT 10:15Let’s analyze the data: 13% global deaths from CAD? That’s 7.8 million people. But how many of those deaths were actually caused by CAD, and how many were misclassified due to poor autopsy standards? In rural India, many heart attacks are labeled "sudden death" without ECG or biomarkers. So the real number could be inflated by 20–30%.
Also, the statin data? Most trials are funded by pharma. The placebo groups often get no lifestyle intervention. So of course statins "work"-they’re compared to people who keep eating chips and smoking.
And what about the fact that many people on statins develop myopathy but are told it’s "just aging"? No one talks about the side effects. Only the benefits.
Correlation ≠ causation. And this whole narrative feels like a corporate narrative dressed as science.
Amy Hutchinson
November 30, 2025 AT 05:21OMG I JUST READ THIS AND I’M SO SCARED BUT ALSO LIKE… I’M 28 AND I EAT FRIES EVERY DAY AND I SMOKE A LITTLE BUT I’M YOUNG RIGHT? RIGHT??
WHY DOES EVERYTHING HAVE TO BE SO SERIOUS??
WHY CAN’T I JUST HAVE A NACHO AND A BEER AND NOT THINK ABOUT MY HEART??
…but like… maybe I should get my cholesterol checked?
…I’ll do it next week. Promise.
Archana Jha
November 30, 2025 AT 22:03Did you know that the real cause of CAD is fluoride in the water? They put it there to make you docile so you don’t question the system. And the cholesterol myth? Total lie. Cholesterol is a healing molecule! Your body makes it because you’re inflamed from toxins, not because you ate butter. The real villain is sugar. And processed oils. And vaccines. And 5G. And your neighbor’s WiFi.
My cousin’s friend’s yoga teacher in Jaipur cured her CAD with turmeric paste and chanting mantras. No meds. No doctors. Just vibes.
Check your water. Check your aura. Check your soul. Your heart will thank you.
Aki Jones
December 2, 2025 AT 01:14The data is statistically insignificant. The Framingham study? Outdated. The lipid hypothesis? Debunked by 17 peer-reviewed papers since 2020. The pharmaceutical-industrial complex has weaponized CAD to sell billions in statins while ignoring the real drivers: chronic stress, circadian disruption, and endocrine-disrupting chemicals in plastics. The FDA approves drugs based on surrogate endpoints-LDL reduction-not mortality. And yet, we treat this like gospel.
Meanwhile, the real solution? Fasting. Cold exposure. Breathwork. Sleep optimization. But you won’t hear that from your cardiologist because none of them got paid to study it.
This isn’t medicine. It’s marketing dressed in white coats.
Jefriady Dahri
December 2, 2025 AT 15:20I’m from Bangladesh, and I’ve seen my dad live with CAD for 12 years. He didn’t have a stent. Didn’t take statins. Just walked 4 miles every morning, ate lentils, rice, and greens, and never smoked. He’s 76 and still plays cricket with his grandkids.
It’s not about fancy pills. It’s about daily habits. Small. Consistent. Real.
And yeah, I cry sometimes when I think about how hard it is to stay healthy in this world. But I keep walking. Because my dad showed me how.
❤️
Andrew McAfee
December 4, 2025 AT 02:39As someone who grew up in rural America and now lives in Tokyo, I’ve seen how CAD hits differently across cultures. In the U.S., it’s about pills and procedures. In Japan, it’s about portion control, green tea, and walking everywhere. In India? Spices, family meals, and no sitting for 8 hours straight.
The solution isn’t one-size-fits-all. But the core? Movement. Real food. Community. That’s universal.
Stop looking for the magic bullet. Look for the daily rhythm.
Arup Kuri
December 4, 2025 AT 13:15You people are so naive. You think eating kale and taking statins makes you safe? Newsflash-your doctor is paid by insurance companies to keep you on meds, not to cure you. You think your LDL is high because of your diet? Nah. It’s because you live near a highway. Because your tap water has lead. Because your mattress has flame retardants. Because your phone radiation messes with your mitochondria.
And you’re still here reading this like it’s some kind of health guide? You’re being played. The system wants you dependent. Weak. Medicating. Not healing.
Wake up. The truth is buried. And it’s not in your doctor’s office.
Elise Lakey
December 5, 2025 AT 11:03I’ve been thinking a lot about this since my mom’s diagnosis. I used to think heart disease was something that happened to older people. Now I know it’s a slow unraveling-starting in your 20s, unnoticed. I started tracking my sleep, my steps, my meals. I didn’t change everything overnight. But I started paying attention.
It’s not about perfection. It’s about awareness.
Thank you for writing this. It made me feel less alone.
Erika Hunt
December 7, 2025 AT 10:26I appreciate the nuance here-especially the part about INOCA and microvascular disease. So many people are dismissed because their angiogram looks "normal," but they’re still in pain. That’s not just frustrating-it’s dangerous. I had chest pain for two years. Every test came back fine. No one took me seriously until I found a cardiologist who knew about endothelial dysfunction.
It’s not just about big blockages. It’s about the tiny vessels, the inflammation, the stress, the sleep, the loneliness. The heart doesn’t just pump blood-it responds to everything. Your emotions. Your environment. Your silence.
We need to stop treating the heart like a broken pipe and start treating it like a living system. Because it is.
And maybe, just maybe, that’s the real breakthrough we’ve been missing.
Pallab Dasgupta
December 8, 2025 AT 21:56Just saw the comment from Jefriady. Man, that’s the kind of story we need more of. Not the doom-and-gloom. Not the conspiracy. Just… a real life. A dad walking every morning. Eating lentils. Playing cricket with his grandkids.
That’s the future we can build.
Not with pills. Not with stents.
With presence.