When you're pregnant and struggling with anxiety or insomnia, the pressure to feel better can be overwhelming. Many women turn to benzodiazepines-medications like lorazepam, diazepam, or alprazolam-because they work quickly and effectively. But what happens when you're carrying a baby? The truth is, these drugs cross the placenta. They don’t just affect you-they reach your developing fetus. And that raises serious questions about safety.
What Are Benzodiazepines, and Why Are They Used in Pregnancy?
Benzodiazepines are a class of drugs first developed in the 1950s. They calm the nervous system, helping with anxiety, panic attacks, muscle spasms, and sleep problems. About 1.7% of pregnant women in the U.S. get prescribed one during the first trimester, and that number is rising. For some, the relief they offer is life-changing-especially when therapy or lifestyle changes aren’t enough.
But here’s the catch: these drugs don’t stay in your bloodstream. They pass through the placenta and build up in fetal tissue. That means your baby is exposed to the same chemicals you’re taking. And while they help you sleep or calm down, they might also interfere with how your baby’s brain, heart, or organs develop.
The Evidence: What Studies Actually Show
Not all studies agree. Some say the risk is small. Others say it’s real-and it’s tied to specific defects.
A 2022 study of over 3 million pregnancies in South Korea found that women who took benzodiazepines in the first trimester had a slightly higher chance of having a baby with a birth defect. The overall risk went up by about 8%. For heart defects specifically, the risk rose by 14%. The more you took each day, the higher the risk. If you were taking more than 2.5 mg of lorazepam-equivalent daily, the chance of a defect climbed even more.
But it’s not just about the total number of defects. Certain rare but serious conditions showed stronger links. The CDC’s National Birth Defects Prevention Study found that alprazolam (Xanax) was tied to a fourfold increase in anophthalmia (missing eyes) and a 2.7 times higher risk of esophageal atresia (a blocked food pipe). Lorazepam was linked to pulmonary valve stenosis-a narrowing of the heart’s main artery.
One defect that kept appearing across studies was Dandy-Walker malformation-a rare brain condition affecting fluid drainage. Women exposed to benzodiazepines had about three times the risk. These aren’t common problems. But when they happen, they change lives.
And then there’s the conflicting data. A 2023 UK study found no clear link between benzodiazepines and birth defects. But here’s the key: that study included women who took these drugs for severe mental illness. It’s possible the underlying condition-not the drug-was driving the risk. That’s called “confounding by indication.” The South Korean study accounted for this by comparing women to themselves over time, and the link still held.
What About Miscarriage and Preterm Birth?
Beyond birth defects, benzodiazepines are linked to other serious outcomes. A 2024 JAMA Psychiatry study found that women taking these drugs during pregnancy had an 85% higher risk of miscarriage. That’s not a small number. Even more concerning: exposure in the 90 days before conception was tied to a higher chance of ectopic pregnancy-a life-threatening condition where the embryo implants outside the uterus.
And it doesn’t stop at birth. Babies exposed to benzodiazepines in the womb are more likely to be born early, weigh less, have low Apgar scores, and need time in the NICU. One study found that for every 1,000 women taking benzodiazepines in the first trimester, about 8 more babies would be born with major defects than in unexposed groups. For heart defects, that number jumps to 14 extra cases per 1,000.
Let’s put that in perspective. The baseline risk of a major birth defect is about 2.87%. With benzodiazepine use, it rises to 3.81%. That’s a 33% increase in relative risk. For most women, that’s still a low absolute risk. But when you’re pregnant, even small increases matter.

Which Benzodiazepines Are Riskiest?
Not all benzodiazepines are the same. Alprazolam (Xanax) keeps popping up in studies as the most concerning. It’s strongly linked to eye and esophageal defects. Diazepam (Valium) and lorazepam (Ativan) are also used, but the data on them is less clear. Some experts believe alprazolam’s faster absorption and shorter half-life might lead to more intense fetal exposure.
Clonazepam and temazepam have been studied less, but there’s no reason to assume they’re safer. If you’re on any benzodiazepine and pregnant, assume it carries some risk. The safest approach? Avoid them entirely in the first trimester unless absolutely necessary.
What Do Medical Guidelines Say?
Here’s the bottom line from major health organizations:
- ACOG (American College of Obstetricians and Gynecologists): Avoid benzodiazepines in the first trimester if possible. Use only for short-term treatment if benefits clearly outweigh risks.
- APA (American Psychiatric Association): Make decisions case by case. Consider the drug, dose, timing, and your mental health needs.
- European Medicines Agency: Avoid during the first trimester unless essential.
- Canadian Guidelines: Generally avoid. Only consider for severe, treatment-resistant anxiety with close monitoring.
The FDA classifies benzodiazepines as Category D-meaning there’s clear evidence of fetal risk. The European and Canadian agencies are even stricter. They don’t just warn-they recommend avoidance.
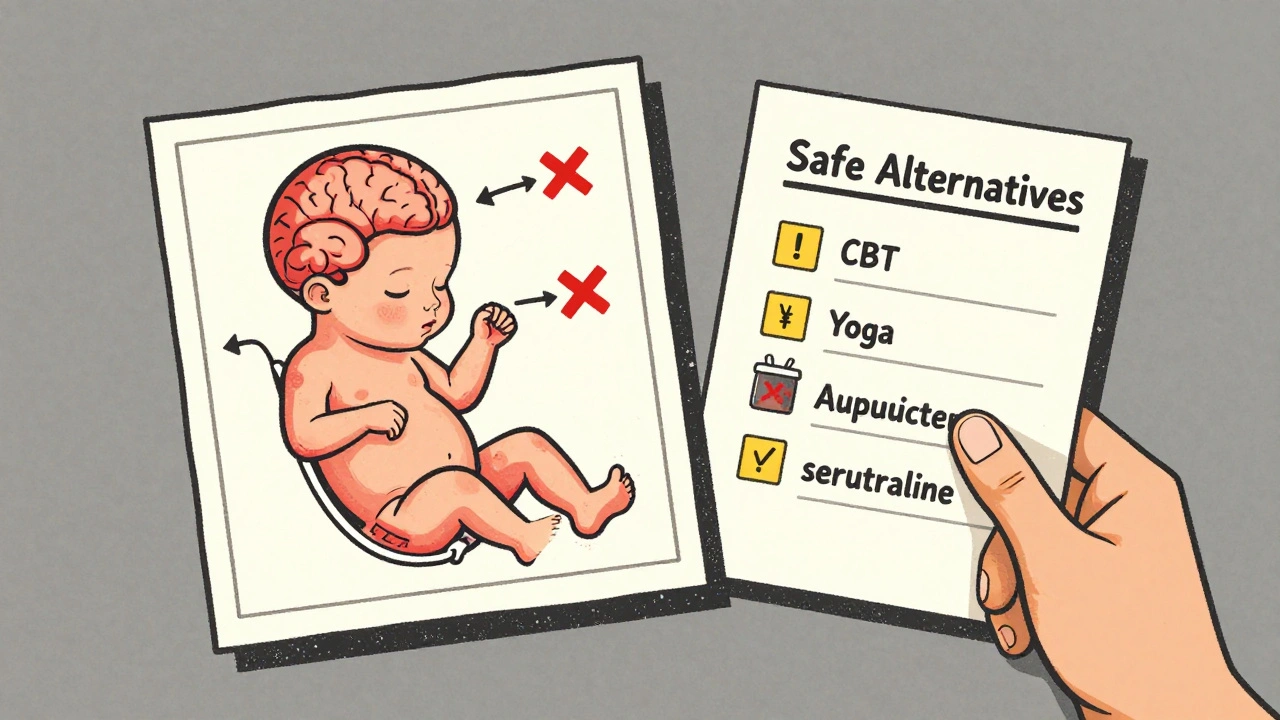
What Are the Alternatives?
If you’re pregnant and anxious or struggling to sleep, you don’t have to go it alone-and you don’t have to take benzodiazepines.
- Cognitive Behavioral Therapy (CBT): Proven effective for anxiety and insomnia during pregnancy. No drugs. No risk.
- Acupuncture: Some studies show it reduces anxiety and improves sleep in pregnant women.
- Mindfulness and yoga: Low-risk, high-reward practices. Many hospitals offer prenatal classes.
- SSRIs (like sertraline): If you need medication, SSRIs are often preferred. Their risk profile is better understood and generally lower than benzodiazepines.
Some women think, “I’ve been on this med for years. I can’t stop.” But stopping suddenly can be dangerous too. Withdrawal can trigger seizures or severe anxiety. That’s why you need a plan-with your OB, psychiatrist, and pharmacist.
What Should You Do If You’re Already Taking Benzodiazepines?
Don’t panic. Don’t quit cold turkey. Do this:
- Call your doctor. Don’t wait for your next appointment.
- Bring your medication list. Include doses and how long you’ve been taking them.
- Ask: “Is this necessary right now? Can we try a safer option?”
- If you’re in the first trimester, the priority is minimizing exposure. A slow taper under medical supervision is safer than abrupt cessation.
- Ask about non-drug therapies. Many are covered by insurance.
And if you’re trying to get pregnant? Talk to your doctor now. Don’t wait until you’re already pregnant. Switching medications or adjusting your treatment plan takes time-and planning.
The Bigger Picture: Mental Health Matters Too
This isn’t about scaring you. It’s about giving you real information so you can make the best choice-for you and your baby.
Untreated anxiety and depression during pregnancy carry their own risks: preterm birth, low birth weight, and long-term developmental issues for the child. If your mental health is collapsing, and nothing else is working, sometimes the risk of staying on a benzodiazepine is lower than the risk of going without treatment.
The goal isn’t perfection. It’s balance. The goal is to get you through pregnancy as safely and healthily as possible. That might mean a lower dose. A different drug. Therapy. Or yes-staying on your current medication, but with careful monitoring.
There’s no one-size-fits-all answer. But there is a clear path forward: talk to your care team. Don’t suffer in silence. Don’t stop cold. Don’t assume it’s safe just because your friend took it and had a healthy baby.
Your body, your baby, your choices. But make them with full information.



Chelsea Moore
December 2, 2025 AT 12:00So let me get this right-you’re telling me that a woman who’s barely holding it together, who’s crying in the shower because she can’t breathe, should just… stop? And what? Do yoga? Really?!!??
Like, I get it-your precious fetus has a 0.94% increased risk of a defect. But what’s the risk of a mother losing her mind? Of her screaming into a pillow at 3 a.m.? Of her not being able to hold her baby when it’s born because she’s a shell of a person?!!
And don’t even get me started on the ‘alternatives.’ CBT? When you can’t even get out of bed? Acupuncture? For $150 a session? And who’s paying for it? Not Medicaid. Not my insurance. Not anyone who actually lives in this country.
You act like this is a choice between ‘perfect baby’ and ‘monster baby.’ But it’s not. It’s between ‘alive, functioning mother’ and ‘broken, suicidal woman who can’t feed herself, let alone a child.’
And now you’re going to tell me to taper? With what? A therapist who doesn’t take my insurance? A doctor who won’t return my calls for three weeks? I’ve been through this. I’ve been the one on Xanax. I’ve had the baby. He’s healthy. He’s 7. He’s brilliant. And I would do it again-in a heartbeat.
So don’t you dare tell me I’m selfish. Don’t you dare tell me I didn’t think about it. I thought about it every single day. And I chose life-for me. And for him.
And if you think you’d do better? Try living in my skin. For one day. Then come back and talk to me about ‘risks.’
John Biesecker
December 2, 2025 AT 17:55Man… this is heavy. 🫠
I read this whole thing and just sat there. Like… we’re talking about real people here. Not stats. Not studies. Real moms. Real panic attacks. Real nights where the only thing that lets you breathe is a little white pill.
And yeah, the data’s scary. But here’s the thing-science doesn’t give us perfect answers. It gives us probabilities. And sometimes, the probability of staying alive is higher than the probability of a perfect baby.
Also… why is it always the mom’s job to be perfect? When’s the last time we talked about the dad’s anxiety meds? Or the dad’s depression? Nobody’s telling him to ‘just meditate’ while his wife cries in the kitchen.
Anyway… just… be kind. To the people taking these pills. And to the ones who can’t.
❤️
Genesis Rubi
December 4, 2025 AT 09:34Oh wow. Another liberal guilt-trip disguised as medical advice.
First, the Koreans did a study? Who cares? Their healthcare system is run by robots. And the CDC? They’re just trying to scare people so they can fund more programs. Meanwhile, in real countries like ours, women make choices. And they’re not stupid.
My cousin took Ativan while pregnant. Baby was born with a full head of hair, 9 pounds, and a PhD in crying at 2 a.m. No defects. No NICU. Just a healthy kid.
Stop pushing your agenda. Let women decide. We’re not lab rats.
Doug Hawk
December 4, 2025 AT 13:32Confounding by indication is the key variable here. The South Korean cohort adjusted for maternal psychiatric burden using within-subject comparisons, which reduces selection bias. But the UK study didn’t stratify by severity of diagnosis-so their null result is likely underpowered for high-risk subgroups.
Also, alprazolam’s pharmacokinetics are unique-high bioavailability, short half-life, rapid placental transfer. That’s why it’s the outlier in teratogenicity data. Not the class.
But here’s the real issue: we’re conflating relative risk with absolute risk. 3.81% vs 2.87% is a 33% increase, yes-but that’s still a 96% chance of no defect.
So the question isn’t ‘is it risky?’ It’s ‘is the risk worth the benefit?’ And that’s a clinical decision. Not a moral one.
Michael Campbell
December 5, 2025 AT 01:42They’re lying. They always lie.
The pharma companies paid for the Korean study. The CDC is in bed with Big Pharma. The FDA’s just trying to sell you SSRIs instead.
My sister took Xanax for 3 months. Had a baby. Baby’s now 12. Plays violin. Top of his class.
They want you scared. So you’ll take their drugs. Their therapy. Their program.
Trust no one.
Fern Marder
December 5, 2025 AT 13:56Chelsea, I hear you. I really do. 🤍
And John, you’re right-it’s not about perfection. It’s about survival.
But I also want to say this: if you’re on benzodiazepines and pregnant, you’re not alone. And you’re not broken. You’re a warrior.
There are so many of us out here, silently taking our pills, terrified we’re hurting our babies, but too exhausted to fight anymore.
You don’t have to be perfect. You just have to be here.
And if you’re reading this and you’re scared? Call someone. Text a friend. Say it out loud.
You’re not failing. You’re fighting.
💛
Shubham Pandey
December 6, 2025 AT 05:40Study says risk. But I don’t care. I took it. Baby fine.
Done.
Elizabeth Farrell
December 6, 2025 AT 07:01I just want to say-this is one of the most compassionate, well-researched pieces I’ve read on this topic in years. Thank you.
For anyone reading this who feels guilty or ashamed-you’re not alone. I’ve been there. I was on lorazepam during my first trimester. I tapered slowly with my OB and psychiatrist. We switched to sertraline. I did CBT. I cried a lot. I felt like a failure.
But I didn’t quit. I didn’t hide. I asked for help.
And my daughter? She’s 4. She loves dinosaurs. She laughs like a bell. She has no birth defects. And I’m so proud of how we got here-not because we were perfect, but because we tried.
You can do this. One step at a time.
You’ve got this.
Sheryl Lynn
December 7, 2025 AT 23:22Oh, darling, the ‘alternatives’ section is just so… quaint.
Acupuncture? Mindfulness? Please. You think a woman who’s having panic attacks in the Target parking lot is going to sit cross-legged and chant ‘om’ while her toddler screams for goldfish?
This reads like a Vogue editorial written by someone who’s never held a crying newborn at 3 a.m. while her husband is working the third shift.
It’s not about ‘choices.’ It’s about survival. And sometimes, survival requires a pill. And a damn good therapist who doesn’t charge $300 an hour.
And no, ‘SSRIs are safer’ isn’t a magic bullet. They’ve got their own risks. But at least they don’t make you feel like a zombie. Which, honestly? Is a win.
Paul Santos
December 8, 2025 AT 11:28It’s fascinating how the discourse around maternal pharmacology has become a moral theater rather than a clinical dialogue. The rhetoric of ‘risk’ is weaponized to enforce normative femininity-where a woman’s body must be a vessel of purity, not a site of medical complexity.
Meanwhile, the structural failures-lack of access to mental healthcare, the collapse of postpartum support, the commodification of wellness-are never addressed.
So we blame the pill. Not the system.
And that, my friends, is the real teratogen.
🙂
Eddy Kimani
December 8, 2025 AT 12:46Just wanted to add-when you’re pregnant and on meds, the scariest part isn’t the birth defects. It’s the silence.
No one talks about this. Not even your OB. Not even your therapist. You Google it at 2 a.m. and feel like a monster.
But here’s what I learned: your mental health IS your baby’s health. A mother who can’t breathe can’t hold her baby. A mother who’s drowning can’t feed her child.
So if you’re taking something to stay alive? That’s not weakness. That’s courage.
And if you’re reading this? You’re not alone.
John Morrow
December 8, 2025 AT 17:46Let’s be honest: this entire article is a product of the ‘medical-industrial complex’ masquerading as maternal care. The 8% increased risk? That’s statistically insignificant when you consider the confounders: maternal age, smoking, alcohol, socioeconomic stress, lack of prenatal care-all of which are far more predictive of birth defects than benzodiazepines.
And yet, we single out one class of drugs because it’s easier to vilify a pill than to fix a broken healthcare system that abandons women after they become pregnant.
The real tragedy isn’t the occasional birth defect. It’s the fact that so many women are left to suffer alone-because we’d rather shame them than support them.
So go ahead. Call me a ‘toxic analyst.’ I’d rather be that than a cheerleader for performative virtue.
Kristen Yates
December 8, 2025 AT 23:25I’m from Kenya. We don’t have benzodiazepines here. We have grandmothers. We have community. We have tea and silence and people who sit with you when you cry.
I moved to the US last year. I had panic attacks. I was scared. I didn’t know what to do.
Then I found a group of moms. We met in a church basement. We didn’t talk about pills. We talked about sleep. About fear. About how hard it is to be a mother here.
Some of us took meds. Some didn’t. We didn’t judge.
Maybe the answer isn’t just pills or yoga.
Maybe it’s each other.
Chelsea Moore
December 9, 2025 AT 17:58Elizabeth-you just said everything I’ve been too angry to say.
I didn’t taper. I didn’t switch. I kept taking it. And I didn’t feel like a monster. I felt like a mother.
Thank you for saying it out loud.