Benzodiazepine Interaction Checker
Check Your Medication Risks
This tool helps you understand the risks of combining benzodiazepines with other common medications and substances. Remember: mixing these drugs can cause dangerous respiratory depression.
Results
When you're overwhelmed by anxiety, a pill that works in under an hour can feel like a lifeline. Benzodiazepines-like Xanax, Ativan, and Valium-are fast, effective, and widely prescribed. But here’s the part no one always tells you: mixing them with other common medications can be deadly. This isn’t hypothetical. It’s happening right now, in homes, ERs, and funeral homes across the country.
How Benzodiazepines Actually Work
Benzodiazepines don’t just calm you down-they slow down your brain. They boost GABA, your body’s main calming neurotransmitter. That’s why they work so quickly: within 30 to 60 minutes, you feel less anxious, more relaxed, sometimes even drowsy. That’s the goal. But that same effect is what makes them dangerous when combined with other substances that also depress the central nervous system.There are three types based on how long they last in your body:
- Short-acting: Alprazolam (Xanax), triazolam (Halcion)-last 6-12 hours. These are the most likely to cause withdrawal and dependence because they leave your system fast.
- Intermediate-acting: Lorazepam (Ativan)-lasts 10-20 hours. Often used for short-term anxiety or before surgery.
- Long-acting: Diazepam (Valium), clonazepam (Klonopin)-can stay in your system for days. Useful for seizure control or tapering off other benzos.
None of them are meant for long-term daily use. The FDA and major medical groups now agree: if you’re taking a benzodiazepine for more than 4 weeks, you’re at serious risk of dependence-even if you’re following your doctor’s instructions.
The Deadly Mix: Benzodiazepines and Opioids
If you’re on painkillers like oxycodone, hydrocodone, or morphine, and your doctor also prescribed you Xanax or Ativan, you’re in a high-risk zone. The numbers don’t lie:- 75% of benzodiazepine-related overdose deaths between 2011 and 2016 involved opioids.
- People taking both have a 15-fold higher chance of fatal overdose than those taking opioids alone.
- In 2019, benzodiazepine-opioid combinations were involved in 23% of all opioid-related deaths.
Why? Both drugs suppress breathing. Alone, opioids can slow your breath. Benzodiazepines make it worse. Together, they can stop it completely-especially during sleep. One Reddit user, u/AnxietyWarrior2020, wrote: “I was on oxycodone for back pain and Xanax for panic attacks. Two weeks in, I stopped breathing at night. They had to revive me in the ER.” That’s not rare. It’s predictable.
The FDA added a Boxed Warning to every benzodiazepine label in September 2020-its strongest safety alert-specifically warning about this combination. Yet, a 2022 AMA survey found only 43% of primary care doctors routinely check for it. That’s not negligence-it’s systemic failure.
Alcohol? Even Worse
You’ve heard “don’t mix alcohol and medication.” But with benzodiazepines, it’s not just a bad idea-it’s a medical emergency. Alcohol isn’t just another depressant. It’s a powerful one. One drink can double the sedative effect. Two drinks? You’re looking at slurred speech, confusion, loss of coordination, and dangerously slowed breathing.Healthgrades analyzed over 1,200 patient reviews. In 27% of negative reviews, people described near-fatal reactions after drinking while on benzos. One wrote: “I had a glass of wine with dinner while on Ativan. I woke up on the floor, couldn’t move, and had no memory of how I got there.” That’s not a blackout-it’s CNS collapse.
There’s no safe amount. Not one beer. Not one glass of wine. Not even a sip. The FDA’s updated medication guides now explicitly say: “Do not drink alcohol while taking this medicine.” And yet, many patients still don’t realize how serious this is.
Other Dangerous Interactions
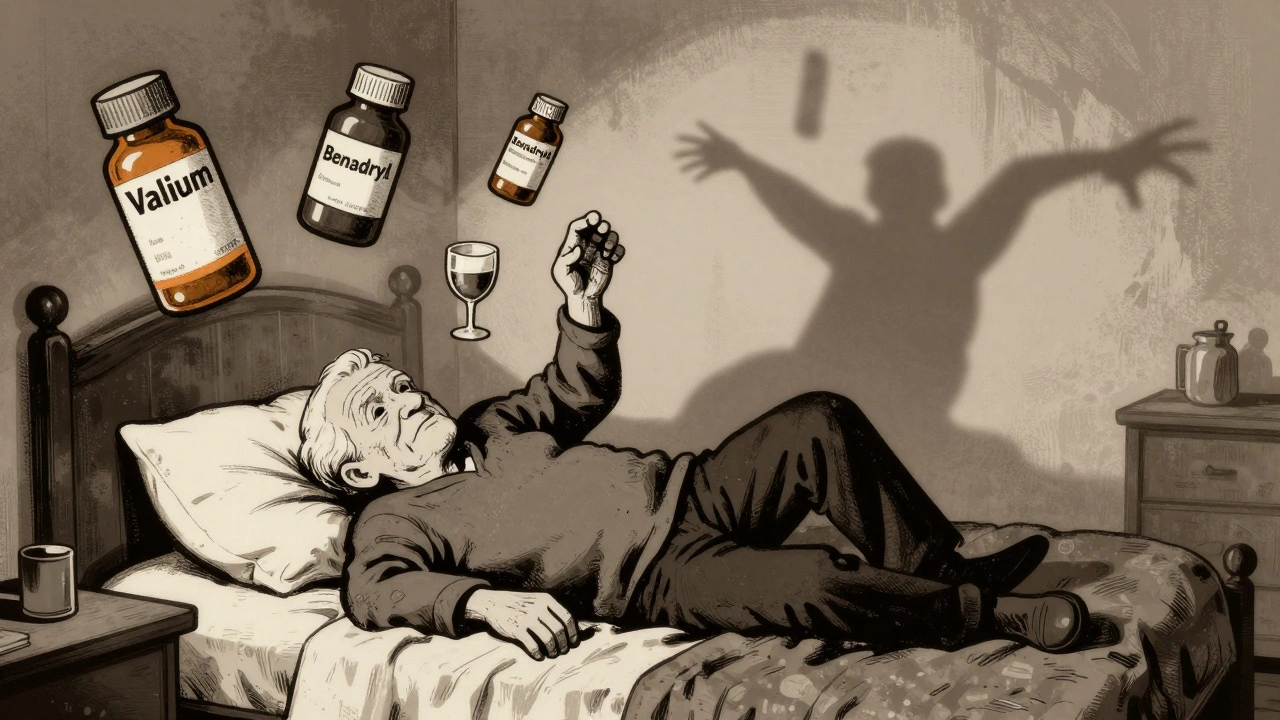
It’s not just opioids and alcohol. Many other medications can turn a benzo into a time bomb:- Sleep meds (Z-drugs): Zolpidem (Ambien), eszopiclone (Lunesta)-these work the same way as benzos. Mixing them increases sedation and overdose risk.
- Antidepressants: While SSRIs like sertraline or escitalopram are safer for long-term anxiety, combining them with benzos can still cause excessive drowsiness, especially in older adults.
- Antihistamines: Diphenhydramine (Benadryl), hydroxyzine-even over-the-counter allergy pills-can add to drowsiness and increase fall risk.
- Muscle relaxants: Cyclobenzaprine, carisoprodol-both are CNS depressants. Used together with benzos, they’re a recipe for respiratory failure.
Older adults are especially vulnerable. The American Geriatrics Society says benzodiazepines should be avoided in people over 65. Why? They’re more sensitive to sedation. Their bodies clear drugs slower. And the risk of falling? It goes up by 50% with benzos alone-and triples when combined with other sedating drugs. A fall at 70 can mean a broken hip, surgery, and never walking again.
Why SSRIs Are the New First Choice
There’s a reason doctors are shifting away from benzodiazepines for long-term anxiety. SSRIs-like fluoxetine, sertraline, and escitalopram-take 4 to 6 weeks to work. But once they do, they’re effective, non-addictive, and safe with most other medications.In 2022, SSRIs were prescribed for 68% of new anxiety cases. Benzodiazepines? Just 22%. That’s not because SSRIs are magic. It’s because they don’t kill.
And unlike benzos, SSRIs don’t require you to stop drinking, avoid pain meds, or fear sleep. They don’t cause withdrawal when you stop. They’re not a quick fix-but they’re a safe long-term solution.

What to Do If You’re Already on a Benzo
If you’re taking a benzodiazepine right now, here’s what you need to do:- Check your full medication list. Go through every pill, patch, and OTC drug you take. Look for opioids, sleep aids, muscle relaxants, antihistamines, and alcohol.
- Don’t stop suddenly. Quitting cold turkey can trigger seizures, hallucinations, or extreme anxiety. Withdrawal from long-term use affects 40% of users.
- Ask for a taper plan. Short-acting benzos (like Xanax) need slower tapers-reduce by 5-10% every 1-2 weeks. Long-acting ones (like Valium) can be cut faster, but still need medical supervision.
- Request a non-benzo alternative. If you’ve been on it for more than a month, ask about SSRIs, SNRIs, or therapy. Cognitive behavioral therapy (CBT) is as effective as medication for anxiety-with no risk of overdose.
- Get your doctor to review your prescriptions. Bring a list to your next appointment. If your doctor doesn’t ask about other meds, ask them: “Could any of these interact with my benzo?”
One patient, who took Ativan for two weeks after surgery while on painkillers, wrote on Drugs.com: “My doctor gave me clear instructions: no alcohol, no extra sleep meds. I followed them. No problems.” That’s the difference between care and negligence.
The Bigger Picture
The U.S. benzodiazepine market is shrinking. Sales dropped from 13.1% of adults in 2013 to 10.8% in 2021. States with prescription monitoring systems saw a 27% drop in dangerous combinations within 18 months. CMS now requires prior authorization for opioid-benzo combos. The FDA’s warnings are finally being heard.But change moves slowly. Millions still get these prescriptions without proper warnings. Still mix them with alcohol. Still don’t realize they’re playing Russian roulette with their breathing.
Benzodiazepines aren’t evil drugs. They’ve helped people survive panic attacks, seizures, and acute trauma. But they’re not for everyday use. And they’re not safe with anything else that makes you sleepy.
If you’re on one, don’t panic. But do act. Talk to your doctor. Review every pill. Say no to alcohol. And if you’re on opioids? Ask if there’s another way to manage your anxiety-because the cost of silence isn’t just discomfort. It’s your life.
Can you die from mixing Xanax and alcohol?
Yes. Mixing Xanax and alcohol can cause severe respiratory depression, leading to unconsciousness, coma, or death. The combination slows your breathing to dangerous levels, especially at night. Even one drink can be risky. The FDA explicitly warns against combining benzodiazepines with alcohol.
How long after taking a benzo can you drink alcohol?
There is no safe window. Benzodiazepines can stay in your system for hours to days, depending on the type. Even if you feel fine, the drug is still active. For short-acting benzos like Xanax, effects last 6-12 hours. For long-acting ones like Valium, they can linger for days. The only safe answer is: never.
Are there any anxiety meds that don’t interact badly with other drugs?
Yes. SSRIs like sertraline (Zoloft) and escitalopram (Lexapro) have minimal dangerous interactions. They don’t cause sedation, dependence, or respiratory depression. They take longer to work-4 to 6 weeks-but are much safer for long-term use and can be combined with most pain medications, sleep aids, and even alcohol (though alcohol still isn’t recommended). Buspirone is another non-addictive option with very few drug interactions.
What should you do if you accidentally mix a benzo with opioids or alcohol?
If you or someone else is drowsy, confused, having trouble breathing, or unresponsive, call emergency services immediately. Do not wait. Benzodiazepine-opioid or benzo-alcohol combinations can cause sudden respiratory arrest. Naloxone (Narcan) can reverse opioid effects but won’t help with benzo overdose alone. Only medical help can manage the full combination.
Is it safe to take a benzo for a few days after surgery?
It can be, if done carefully. Short-term use (2-4 days) under medical supervision, with clear instructions to avoid alcohol and other sedatives, is sometimes appropriate. Many patients use lorazepam (Ativan) briefly after surgery for anxiety or to help with sleep. But if you’re already on opioids, pain meds, or sleep aids, your doctor must adjust dosages or avoid benzos entirely. Always ask: “Is this necessary, and what are the risks with my other meds?”
Can you get addicted to benzodiazepines even if you take them as prescribed?
Yes. Physical dependence can develop in as little as 2-4 weeks, even when taken exactly as directed. That’s why guidelines now limit use to 4 weeks or less. Dependence means your body adapts to the drug, and stopping suddenly causes withdrawal symptoms-ranging from anxiety and insomnia to seizures. Addiction involves compulsive use despite harm. Both are real risks, even with a prescription.



Anthony Breakspear
December 3, 2025 AT 06:15Man, I’ve been on Xanax for three years after my dad passed. Didn’t realize I was one glass of wine away from not waking up. This post hit me like a brick. Thanks for laying it out like this - I’m scheduling a taper plan with my doc next week. No more drinking. No more excuses.
Zoe Bray
December 3, 2025 AT 18:23It is imperative to underscore that the concomitant administration of benzodiazepines with central nervous system depressants constitutes a Class I pharmacological contraindication, per the FDA’s 2020 Boxed Warning and subsequent AMA clinical guidelines. The synergistic respiratory depression observed in polypharmacy cases is not merely a statistical anomaly-it is a preventable iatrogenic catastrophe.
Girish Padia
December 4, 2025 AT 16:24You people just take pills like candy. Back in India, we deal with anxiety with yoga, chai, and silence. No drugs. No drama. Just discipline. You think your brain is too weak? Maybe it’s your lifestyle.
Saket Modi
December 6, 2025 AT 06:56lol another fear-mongering medical post. I take Xanax and whiskey every Friday. I’m fine. 😴
Chris Wallace
December 6, 2025 AT 12:26I’ve been on Ativan for 18 months now, and I’ve never felt more stable. But reading this made me realize I never asked my doctor about my muscle relaxant or that sleep aid I got from the ER. I’ve been taking them together for months. I didn’t think they’d interact. I’m scared. I’m making an appointment tomorrow. I just needed someone to say it out loud.
william tao
December 7, 2025 AT 20:02Another example of modern medicine’s abject failure. You prescribe a drug that is inherently addictive, then act shocked when people misuse it. The real problem? We’ve outsourced emotional resilience to pharmaceutical corporations. The solution isn’t SSRIs-it’s accountability. And therapy. And a damn culture that doesn’t treat anxiety like a vending machine malfunction.
Shubham Pandey
December 8, 2025 AT 12:57Stop taking benzos. Use SSRIs. Done.
Elizabeth Farrell
December 10, 2025 AT 07:51I want to say thank you to whoever wrote this. I’ve been terrified to tell anyone I’m on Klonopin because I feel so guilty. I thought I was weak for needing it. But now I see-this isn’t about weakness. It’s about safety. I’m going to talk to my doctor about switching to sertraline. And I’m cutting out wine. Not because I’m being dramatic-but because I want to be here for my kids. You gave me courage.
Sheryl Lynn
December 10, 2025 AT 21:36How quaint. You’re all treating benzodiazepines like some kind of tragic Shakespearean flaw. In reality, they’re just poorly understood pharmacological tools. SSRIs? Overrated. The real issue is the lack of neurochemical literacy among primary care providers. If we had more psychopharmacology-trained GPs, we wouldn’t be having this conversation. We’d be optimizing regimens. Not panicking.
Paul Santos
December 11, 2025 AT 16:08There’s a certain poetic tragedy in our age: we’ve mechanized the soul into a neurotransmitter equation. Benzodiazepines are not the enemy-they’re the symptom. We’ve created a world where stillness is unbearable, so we chemically mute the noise. But silence isn’t peace. It’s just chemical stillness. And when you stop… the noise comes back louder. 🤔
Eddy Kimani
December 12, 2025 AT 03:15Interesting data point: SSRIs have a 68% prescription rate for new anxiety cases. But what’s the discontinuation rate? And how many patients report functional improvement? We’re conflating prescription volume with efficacy. Also, CBT is great-but access is wildly uneven. Not everyone can afford 20 sessions. We need scalable, evidence-based alternatives. Not just brand-name pills.
Chelsea Moore
December 12, 2025 AT 16:01THIS IS WHY WE CAN’T HAVE NICE THINGS!! My cousin died from mixing Xanax and Ambien!! And now they’re giving it to teenagers like candy!! My sister’s therapist said it was “fine”!! I’m so angry!! I’m so heartbroken!! I’m so sick of doctors not caring!!
John Biesecker
December 12, 2025 AT 16:11man i’ve been on valium for 6 years and i still ride my bike to work. i don’t drink, i don’t mix, i just take my dose. i think the real issue is that people don’t know how to use these things right. it’s like giving someone a chainsaw and saying “be careful” 😅
Anthony Breakspear
December 13, 2025 AT 13:19Just got off the phone with my doctor. They agreed to switch me to Lexapro. Also said I should cut out my muscle relaxant. I didn’t even realize I was taking two CNS depressants. Thanks for the nudge, everyone. I’m not alone in this.